Introduction
- From staff shortages to reimbursement cuts, a wide range of challenges continue to strain the U.S. health care system. These issues have put increasing pressure on physicians across the country.
- As the leading digital platform for U.S. medical professionals, with over 80% of U.S. physicians as members, Doximity maintains one of the most comprehensive data sets for physician compensation.
- Average physician compensation in the U.S. increased 3.7% from 2023 to 2024, a slightly lower increase than the 5.9% reported in the prior year. This modest growth comes amid several consecutive years of reimbursement cuts—a trend that many physicians worry could impact their ability to care for Medicare and Medicaid patients in the near future.
- Many physicians also believe that current reimbursement policy has contributed to the steady decline of independent practices in their fields. According to the American Medical Association, the share of physicians working in private practices dropped by 18 percentage points—from 60.1% to 42.2%—between 2012 and 2024.1
- Compounding these financial pressures is a growing demand for care and an ongoing shortage of physicians. These challenges have led the majority of physicians surveyed to report being overworked, with more than two-thirds now looking for an employment change or considering early retirement.
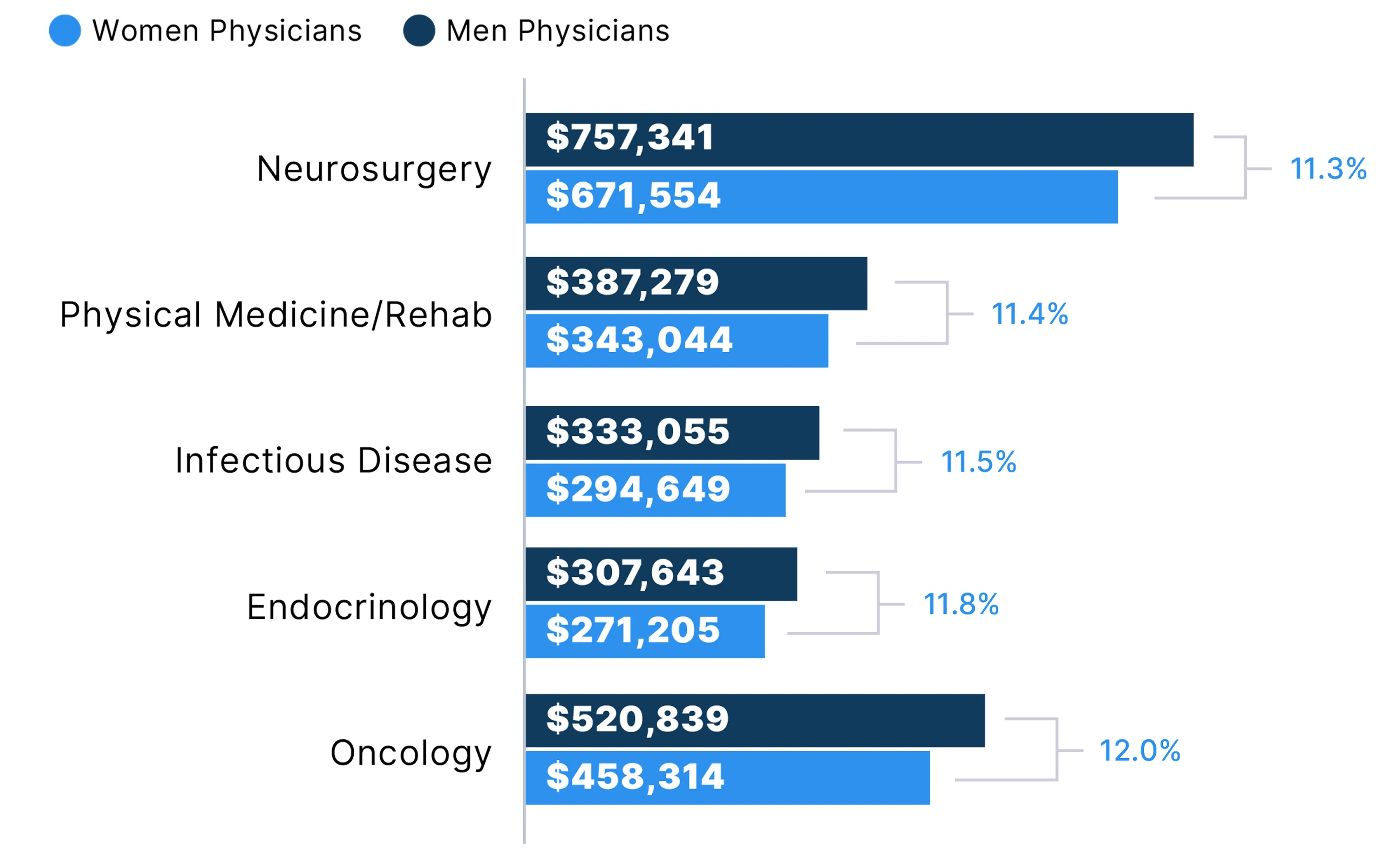
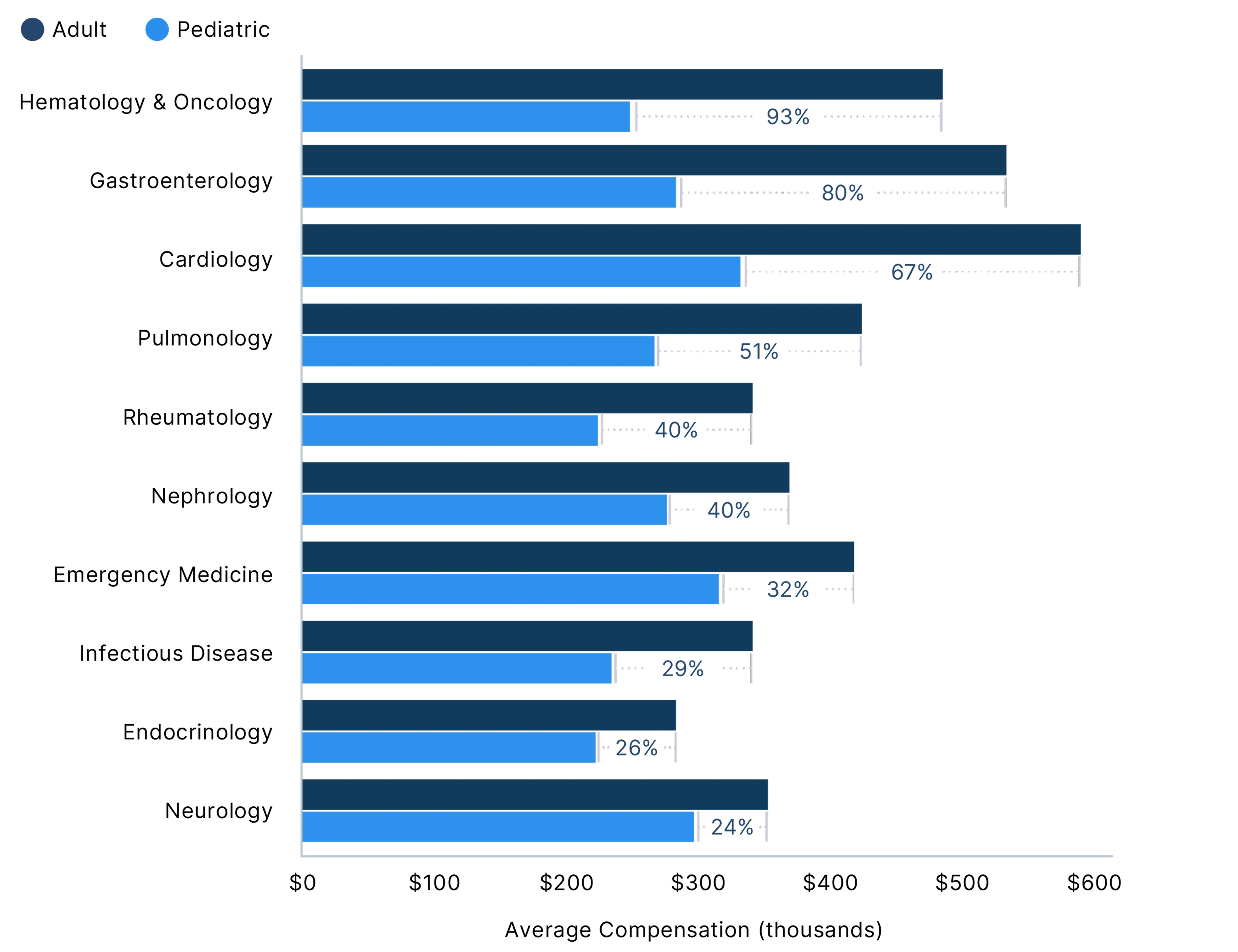
- Further, the 3.7% increase in compensation has done little to close existing pay gaps across the profession. In 2024, average compensation for men rose 5.7%, compared with just 1.7% for women—widening the gender pay gap to 26%, compared with 23% in 2023. Significant disparities also persist between physicians who care for adult versus pediatric patients. In some specialties, the pay gap between pediatric and adult specialists exceeded 80%, despite similar levels of training and clinical complexity.
- This year’s compensation findings draw from approximately 230,000 survey responses over six years, including responses from more than 37,000 U.S. physicians in 2024 alone. The report also incorporates thousands of physician responses to additional surveys and polls fielded throughout 2024 and 2025, as well as data from Doximity’s tech-enabled Talent Solutions, which support both permanent and locum tenens healthcare staffing.
- Together, these insights aim to give physicians a clearer understanding of the compensation landscape and the broader challenges facing the workforce today. Greater awareness of these trends may help physicians make more-informed career decisions and more effectively advocate for both themselves and the patients who need them.
Metro Areas
Compensation by Metro Area
Average Physician Compensation Up 3.7%
Average physician compensation in the U.S. increased 3.7% from 2023 to 2024, a slightly lower increase than 5.9% in the prior year. The metropolitan area with the highest average physician compensation in 2024 was Rochester, MN. As a small market anchored by a leading medical system, Rochester saw an annual growth rate of 8.7%—one of the largest increases in physician compensation this year.
Among the ten metropolitan areas with the highest average compensation in 2024, half are located in the state of California. All but one of the top ten, San Jose, CA, saw a positive increase in compensation. Eight of the ten metropolitan areas with the lowest average compensation are located on the East Coast.
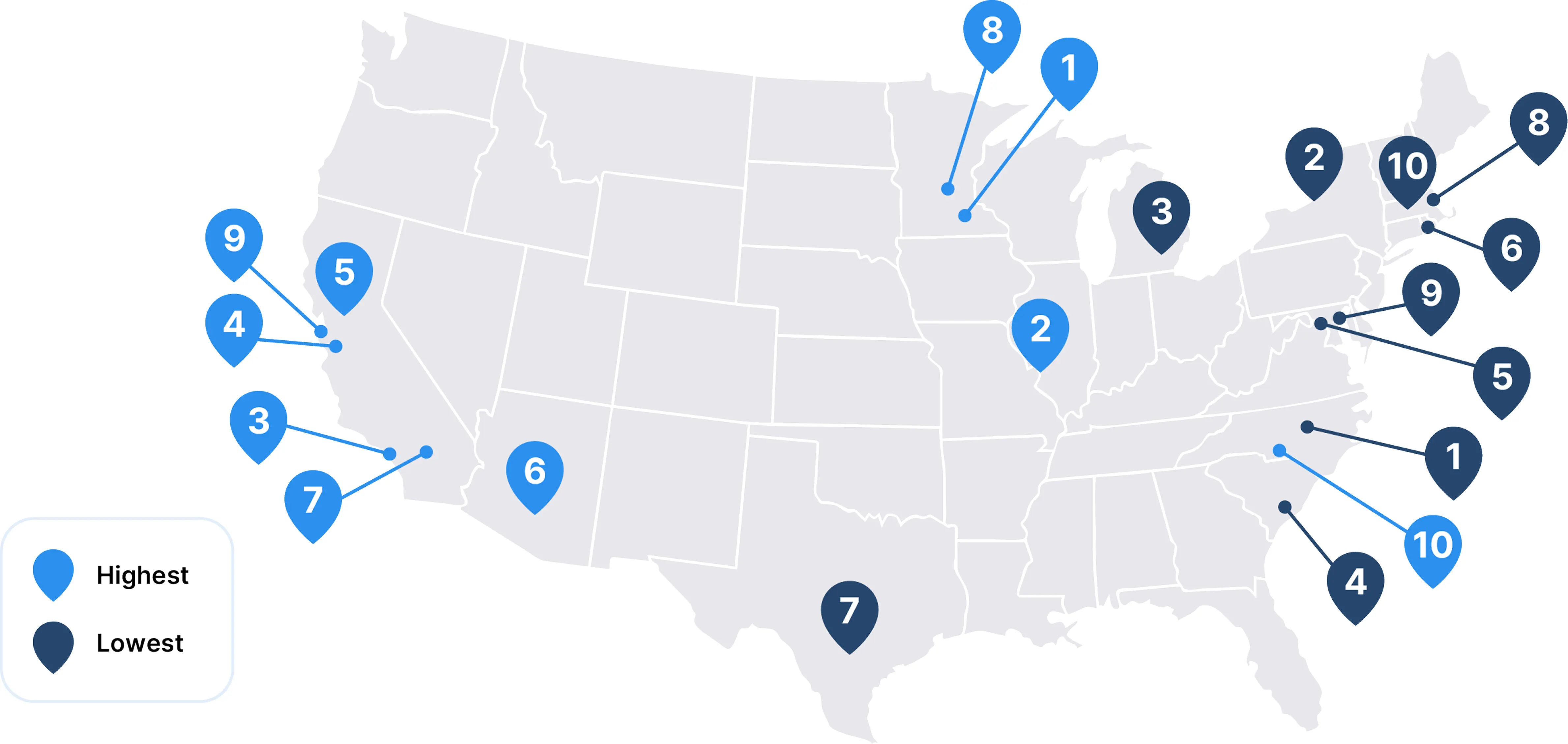
Metro Areas with the HIGHEST Average Physician Compensation
| Metro Area | Average Compensation |
|---|---|
| 1. Rochester, MN | $495,532 |
| 2. St. Louis, MO | $484,883 |
| 3. Los Angeles, CA | $470,198 |
| 4. San Jose, CA | $469,878 |
| 5. Sacramento, CA | $460,671 |
| 6. Phoenix, AZ | $459,082 |
| 7. Riverside, CA | $455,986 |
| 8. Minneapolis, MN | $452,598 |
| 9. San Francisco, CA | $449,830 |
| 10. Charlotte, NC | $448,400 |
Metro Areas with the LOWEST Average Physician Compensation
| Metro Area | Average Compensation |
|---|---|
| 1. Durham-Chapel Hill, NC | $358,782 |
| 2. Rochester, NY | $364,160 |
| 3. Ann Arbor, MI | $373,154 |
| 4. Charleston, SC | $384,419 |
| 5. Washington, DC | $386,731 |
| 6. Providence, RI | $386,788 |
| 7. San Antonio, TX | $389,495 |
| 8. Boston, MA | $390,799 |
| 9. Baltimore, MD | $392,507 |
| 10. Worcester, MA | $397,188 |
Pay Rankings After Cost of Living
Rochester, MN Maintains Top Spot After Cost-of-Living Adjustment
While physicians overall saw an increase in average compensation in 2024, cost of living continues to be a major factor shaping real income. Rochester, MN secured the #1 spot this year for highest compensation adjusted for cost of living, climbing ahead of St. Louis and Oklahoma City. Several metro areas, including St. Louis, Oklahoma City, Charlotte, and New Orleans, remained in the top tier from last year, reflecting a combination of competitive physician pay and relatively affordable living costs.
On the other end of the spectrum, metro areas with the lowest adjusted compensation continue to be concentrated along the East and West Coasts. Boston and Washington, DC once again topped this list, joined by cities like Seattle, San Francisco, and Denver, where higher living expenses continue to erode physician earning power despite nominal pay increases.
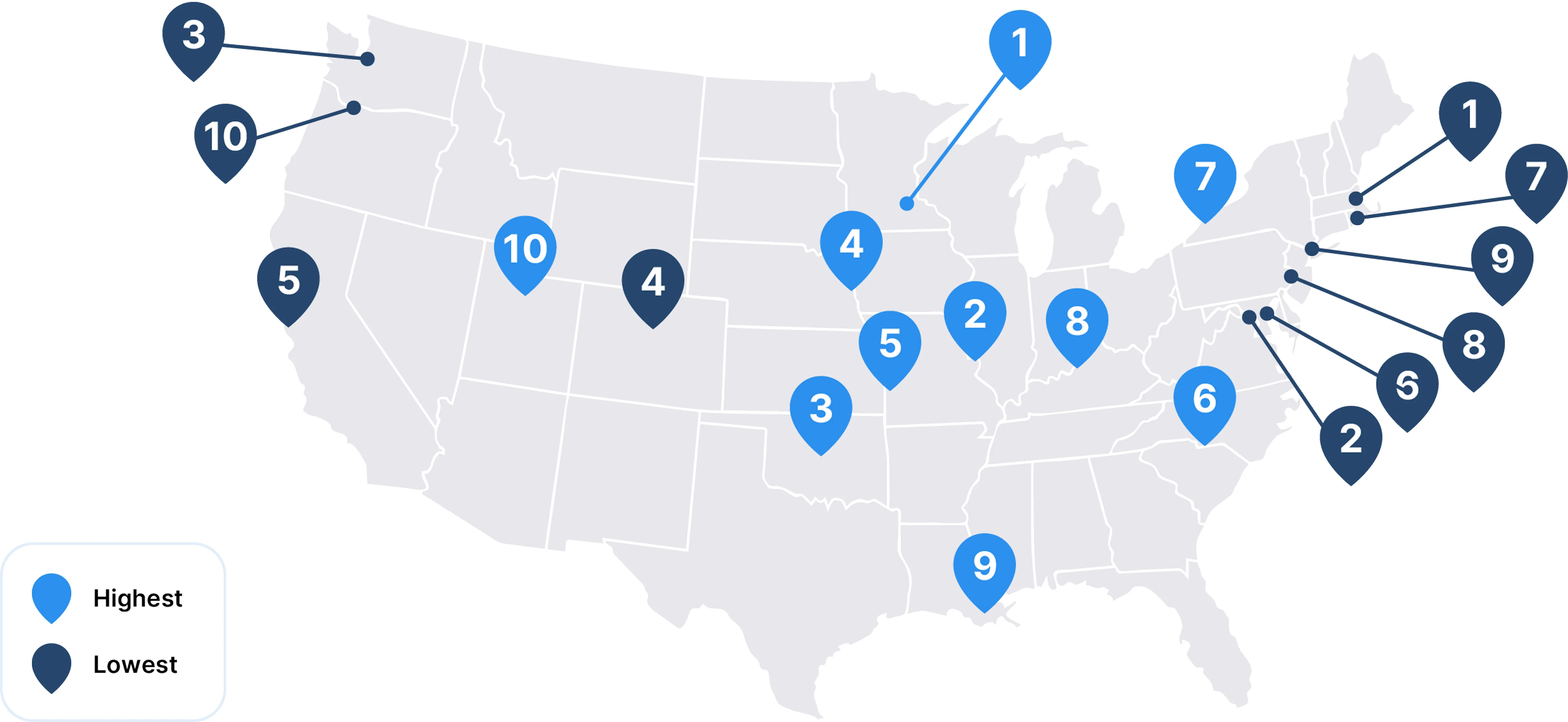
HIGHEST Average Compensation Adjusted for Cost of Living
| Metro Area |
|---|
| 1. Rochester, MN |
| 2. St. Louis, MO |
| 3. Oklahoma City, OK |
| 4. Omaha, NE |
| 5. Kansas City, MO |
| 6. Charlotte, NC |
| 7. Buffalo, NY |
| 8. Louisville, KY |
| 9. New Orleans, LA |
| 10. Salt Lake City, UT |
LOWEST Average Compensation Adjusted for Cost of Living
| Metro Area |
|---|
| 1. Boston, MA |
| 2. Washington, DC |
| 3. Seattle, WA |
| 4. Denver, CO |
| 5. San Francisco, CA |
| 6. Baltimore, MD |
| 7. Providence, RI |
| 8. Philadelphia, PA |
| 9. New York, NY |
| 10. Portland, OR |
Compensation Growth by Metro Area
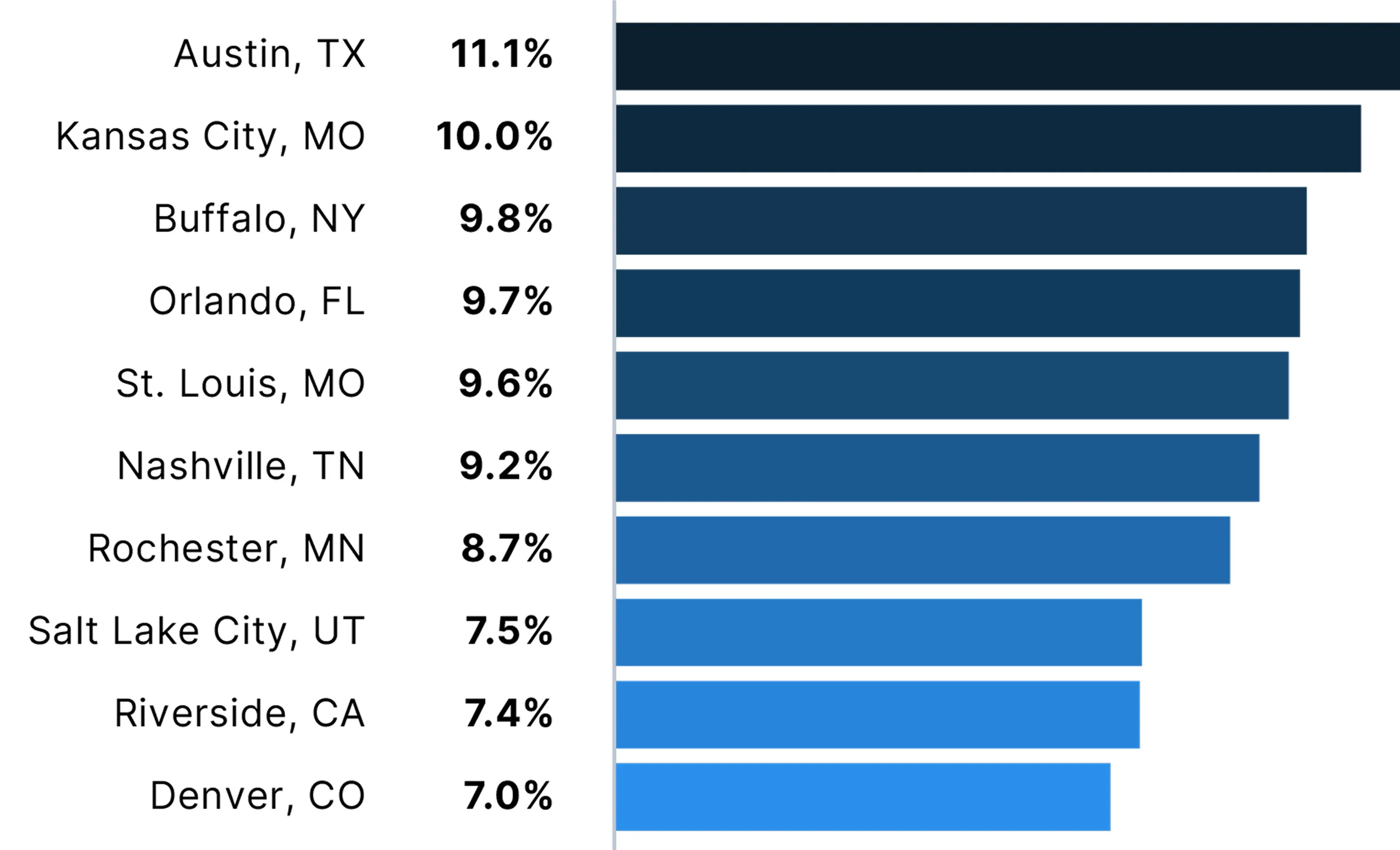
Nearly All Metro Areas Saw Compensation Go Up
Average physician compensation went up in 54 out of the 60 metropolitan areas examined, with about two-thirds seeing growth of at least 3%. The strongest growth was spread across the U.S., with all four major regions represented in the top 10 metro areas.
While the inflation rate in 2024 returned closer to pre-pandemic levels, physicians are still feeling the effects of several years of high inflation—including 7% in 2021 and 6.5% in 2022—and ongoing Medicare payment cuts, including another 2.8% cut in 2025.2,3 According to the American Medical Association, Medicare physician payment has dropped 33% since 2001, after adjusting for inflation.4
This environment underscores that, for many physicians, real earnings have not kept pace with rising costs and declining payment rates.
Specialty & Practice Setting
Compensation by Specialty
Adult Surgical and Procedural Specialties Remain Ahead in Average Compensation
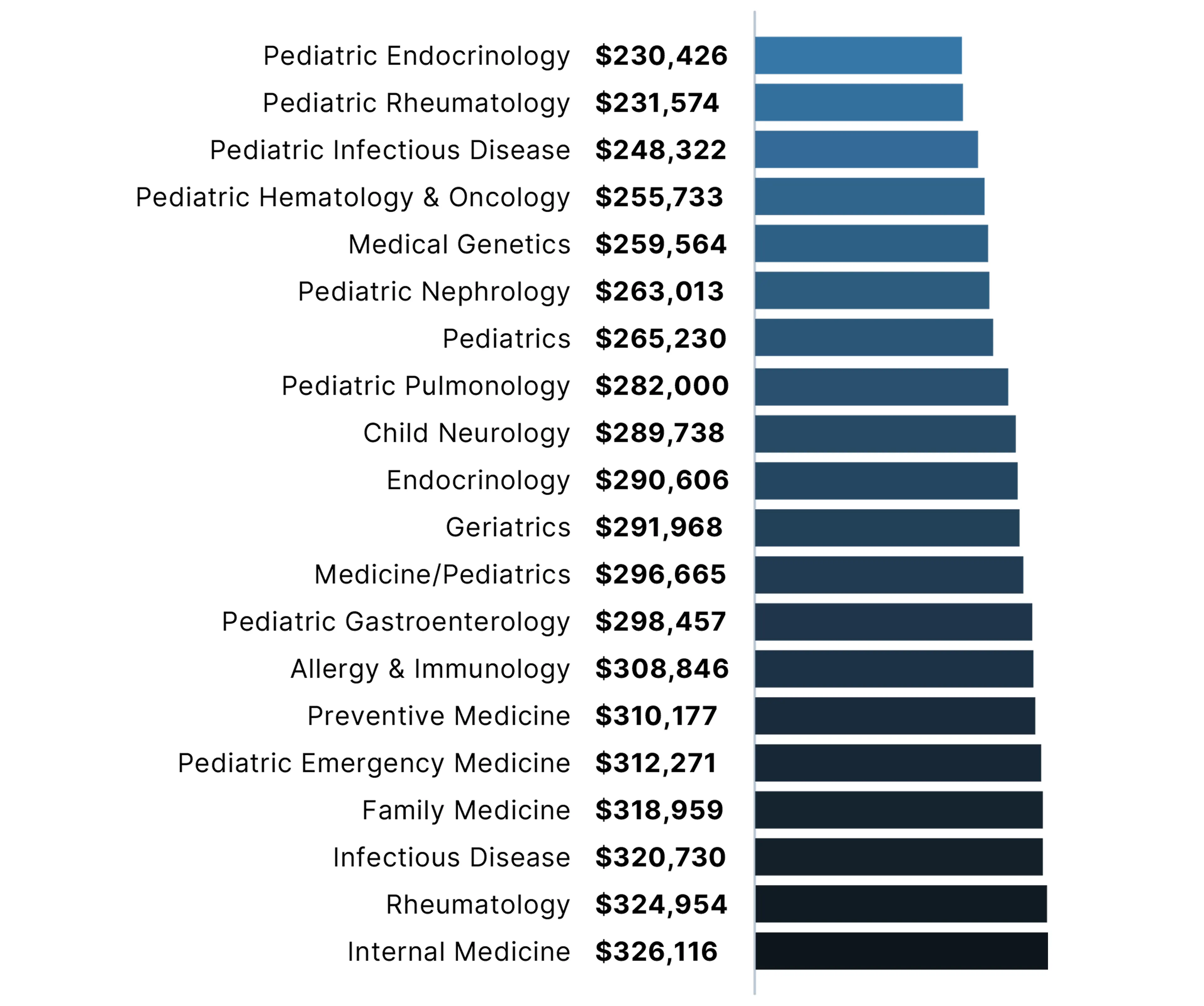
The 20 specialties with the HIGHEST average annual compensation tend to be surgical and procedural specialties
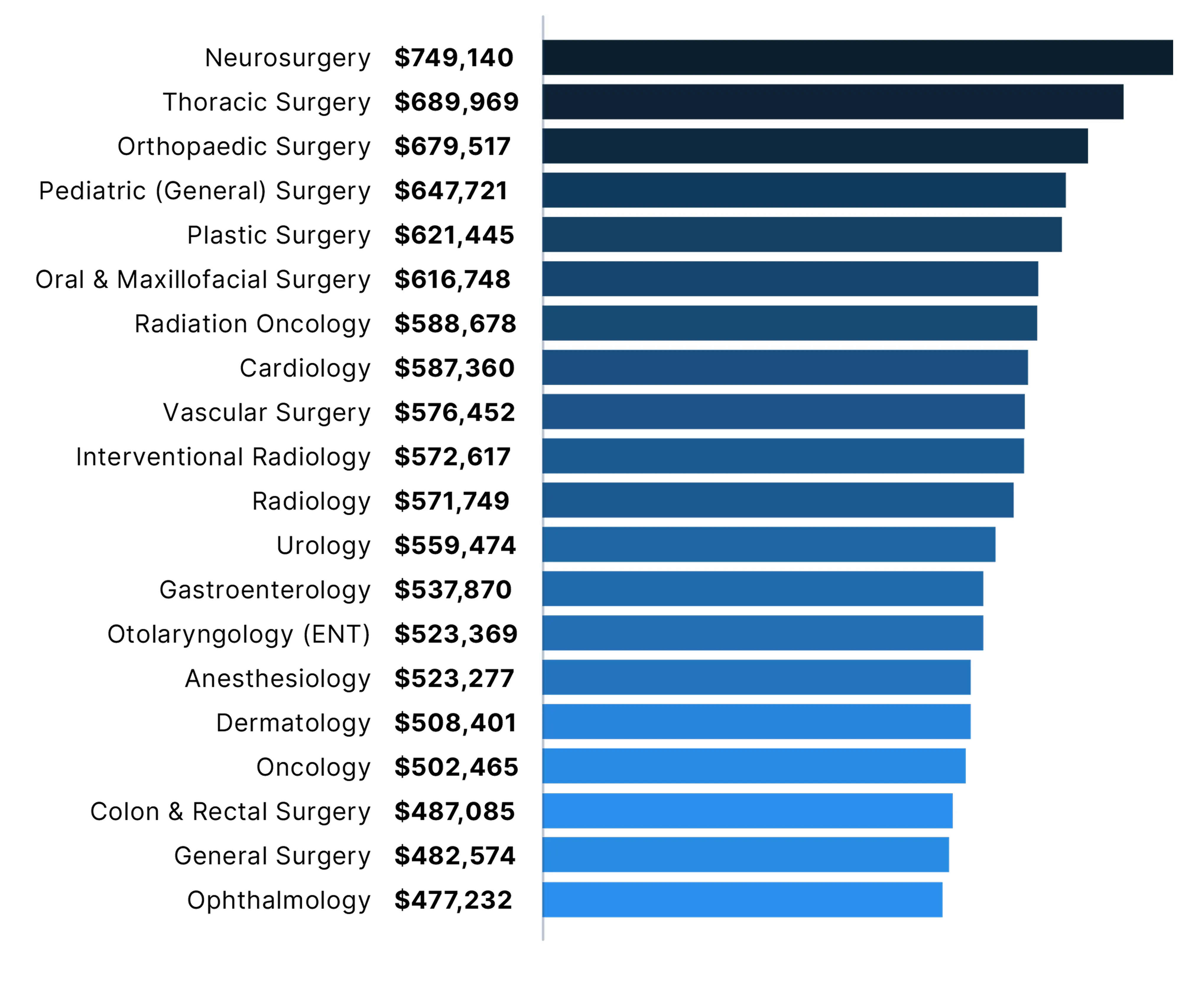
The 20 specialties with the LOWEST average annual compensation tend to be pediatric and primary care specialties
Compensation Growth by Specialty
Pediatric Nephrology, Preventive Medicine See Double-Digit Growth
In 2024, average annual compensation rose for nearly all specialties. The top 10 specialties with the largest increase reported annual growth rates of about 6% or higher. In comparison, the top 10 average annual growth rates in 2023 all exceeded 7%.
The 10 specialties with the largest growth in 2024 include a combination of primary care specialties and surgical and procedural specialties. They also include specialties that were among both the 20 highest and 20 lowest in physician compensation.
Pediatric nephrologists reported a 15.6% growth in compensation, the highest among all individual specialties reviewed in 2024. This increase comes amid concerns over a workforce shortage in a historically small specialty, which has seen trainee interest decline over the past two decades, as well as rising prevalence of childhood obesity and chronic kidney disease.5,6 Research shows that nephrology is one of the pediatric subspecialties with the largest workforce shortages in the U.S.7
The top 10 specialties with the LARGEST increase in average annual compensation
| Specialty | Compensation Growth | Average Compensation |
|---|---|---|
| Pediatric Nephrology | 15.6% | $263,013 |
| Preventive Medicine | 10.0% | $310,177 |
| Medicine/Pediatrics | 8.5% | $296,665 |
| Radiology | 7.5% | $571,749 |
| Hematology | 7.4% | $421,482 |
| Colon & Rectal Surgery | 7.0% | $487,085 |
| Rheumatology | 6.4% | $324,954 |
| Medical Genetics | 6.2% | $259,564 |
| Family Medicine | 6.0% | $318,959 |
| Anesthesiology | 5.8% | $523,277 |
Compensation Gap Between Primary Care and Other Specialties
Pay Differences Remain Wide, Though Gaps Have Narrowed
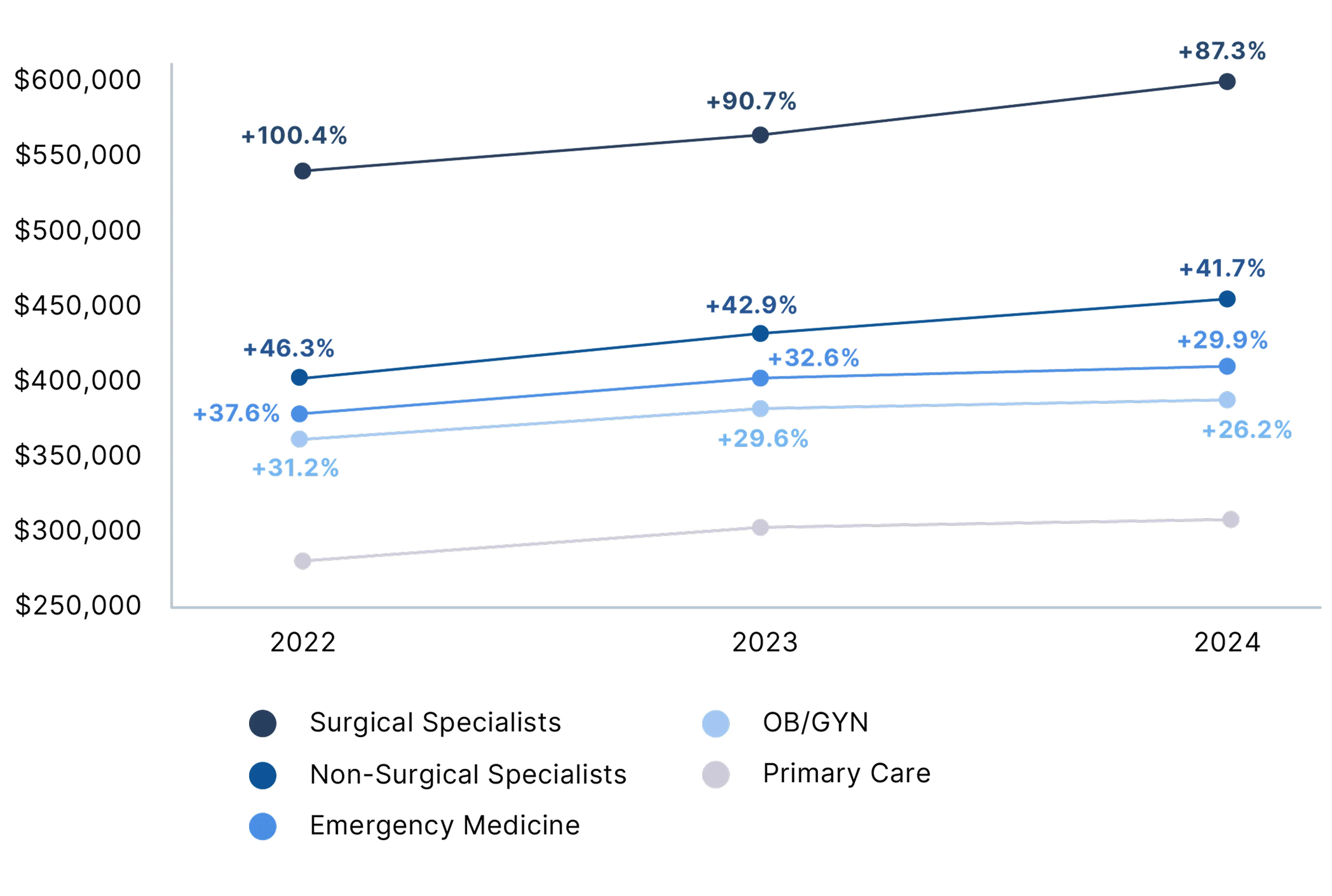
Over the past three years, the percent pay gap between primary care physicians and specialists has declined modestly. In 2024, surgical specialists earned 87% more than primary care physicians, down from 100% in 2022. Non-surgical specialists, emergency medicine physicians, and OB/GYNs also continued to earn significantly more than primary care physicians, though the gaps have narrowed slightly.
These trends come at a time when primary care remains critical to meeting high patient demand, especially amid ongoing physician shortages. While the pay gap is narrowing slightly, primary care physicians continue to earn considerably less than many of their medical colleagues despite their essential role in the health care system.
Average Physician Compensation by Specialty Type (2022-2024)
(+% = Amount Earned Over Primary Care Compensation)
Compensation by Employment Setting
Single Specialty, Multi-Specialty Groups and Solo Practices Continue to Lead
Physician compensation varied widely by practice setting, with single specialty groups, multi-specialty groups, and solo practices providing the highest average annual compensation after adjusting for specialty, location, and years of experience. Average physician compensation increased across all settings in 2024, with urgent care centers showing the highest growth at 6.7%.
Physician Compensation by Practice Setting
| Practice Setting | Average Compensation |
|---|---|
| Single Specialty Group | $476,807 |
| Multi-Specialty Group | $461,671 |
| Solo Practice | $457,562 |
| Hospital | $439,319 |
| Health System / IDN / ACO | $438,983 |
| Health Maintenance Organization | $411,687 |
| Industry | $396,059 |
| Academic | $382,223 |
| Hospital/System - Ambulatory | $370,278 |
| Urgent Care Center / Chain | $307,768 |
| Government | $303,385 |
Gender Pay Gap
Physician Gender Pay Gap
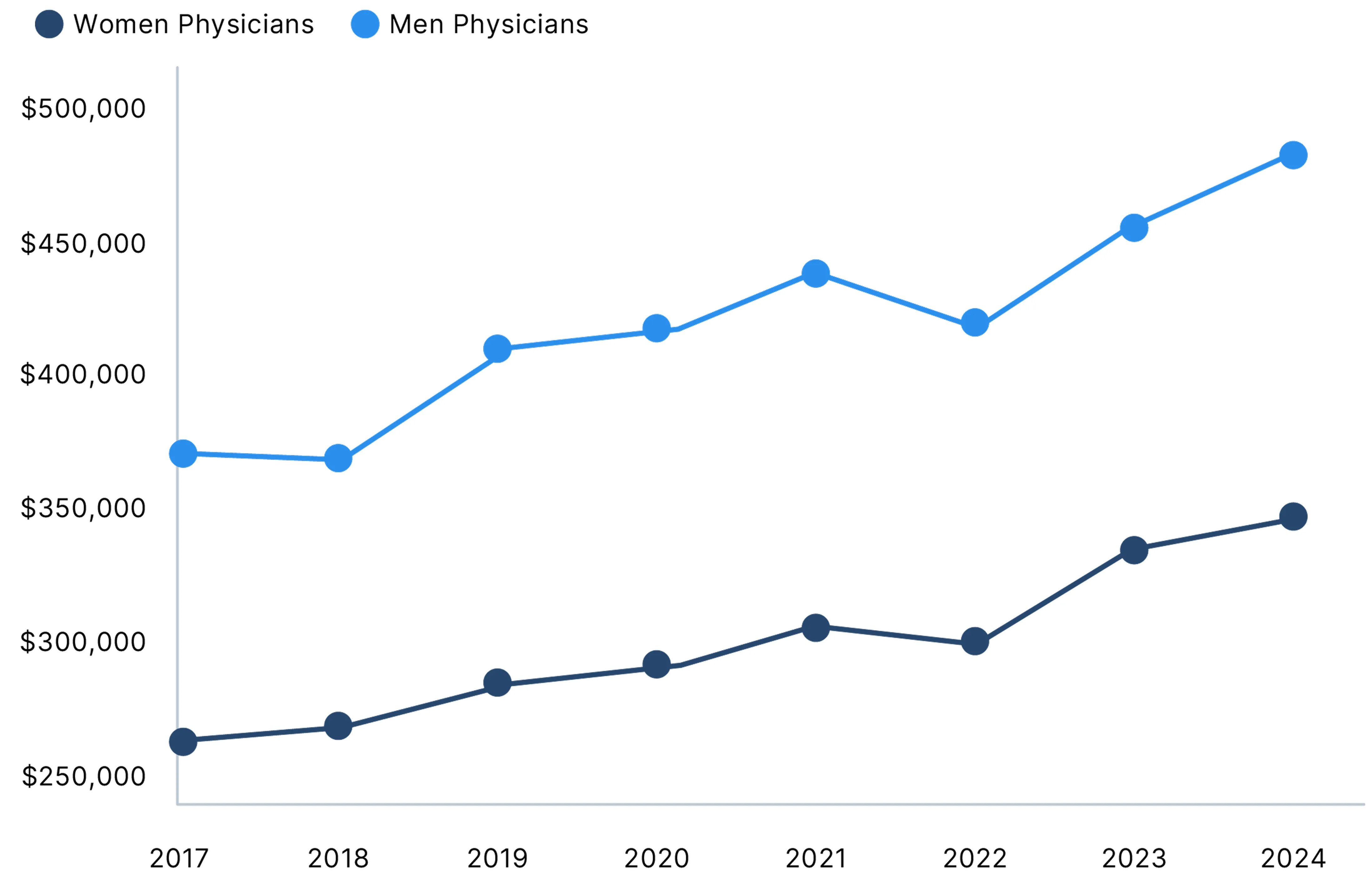
Gender Pay Gap Returns to 26%
The gender pay gap for physicians reached 26% in 2024, up from 23% in 2023 and matching the level seen in 2022. A key contributor was the difference in annual compensation growth: men's pay rose 5.7% in 2024, while women’s increased just 1.7%.
On average, women physicians earned $120,917 less than men physicians after adjusting for specialty, location, and years of experience.
An analysis of our physician compensation data from 2014-2019 estimated that, on average, men make over $2 million more than women over the course of a 40-year career.8
Physician Average Annual Compensation
Physician Gender Pay Gap by Specialty
Men Report Higher Compensation Than Women in All Specialties
Women physicians had lower average earnings than men physicians across all specialties examined in 2024, a trend consistent with prior years. The gender pay gap exceeded 11% in each of these specialties.
The largest gender pay gap as a percentage of pay was in pediatric nephrology, which saw the largest annual growth in pay. Oncology, in contrast, was one of the five specialties with the smallest gender pay gaps, as in 2023.
Medical Specialties with the LARGEST Pay Gaps in 2024
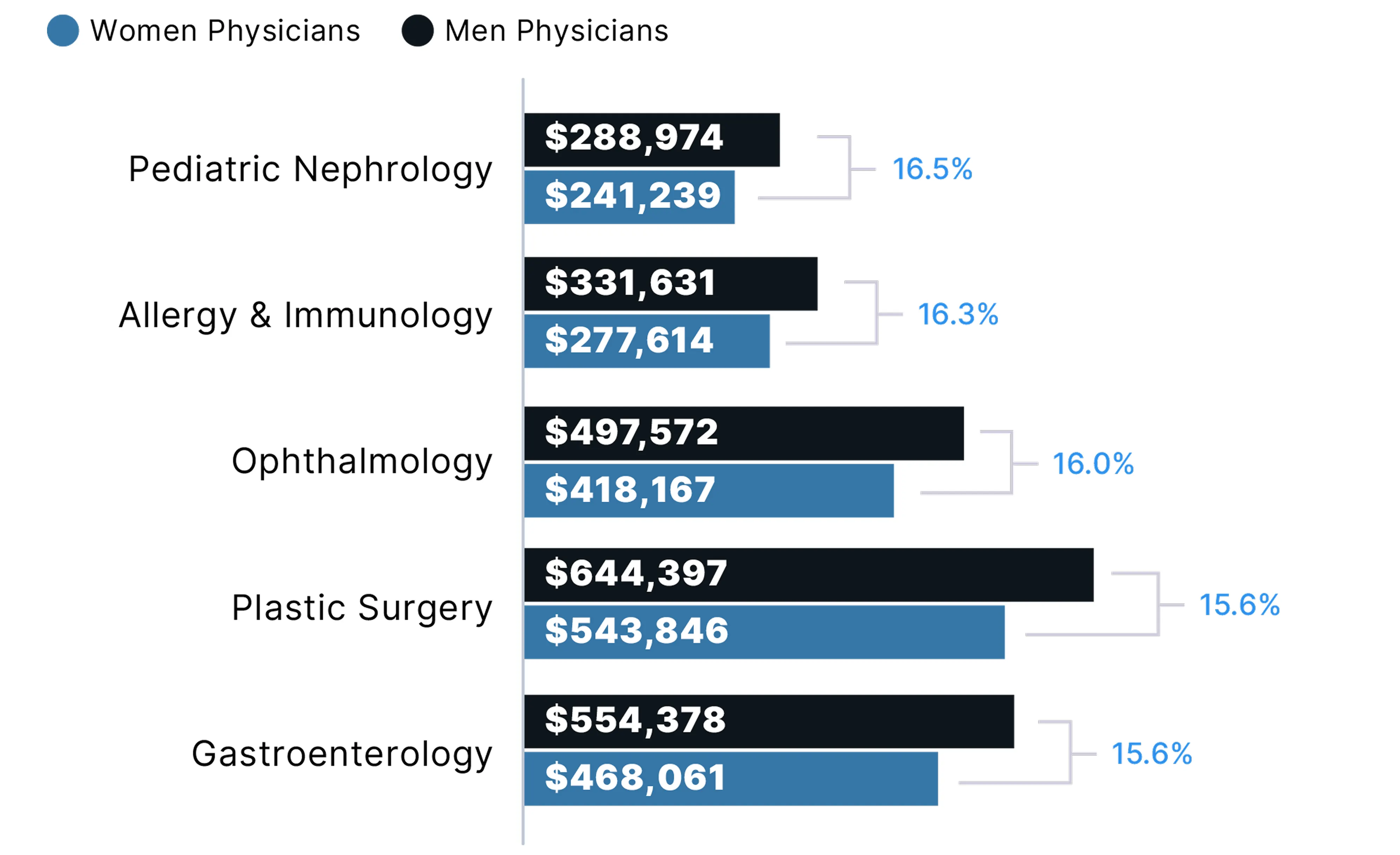
Medical Specialties with the SMALLEST Pay Gaps in 2024
Pediatric Pay Gap
Pediatric Pay Gap by Specialty
Pediatric Specialists Earn Significantly Less Than Their Adult Medicine Counterparts
In 2024, pediatric specialists across all fields examined earned considerably less than adult medicine specialists, despite similar levels of training and responsibility. The largest gaps were seen in hematology and oncology, where adult specialists earned 93% more than their pediatric peers, and gastroenterology, with an 80% pay gap. Cardiology, pulmonology, and rheumatology also showed substantial differences in pay. These gaps appear to reflect a systemic lag in pay for pediatric specialty care, even as demand for pediatric subspecialists continues to rise.
The persistence of these pay gaps is especially concerning given the critical role pediatric subspecialists play in managing complex and chronic conditions in children. In addition, these gaps risk contributing to further workforce shortages, longer patient wait times, and greater challenges in accessing care—especially in underserved areas.
With many pediatrics departments having low profit margins or no margins at all, research shows that they are facing a crisis. To address this issue, there is a continued need for parity between Medicaid and Medicare payment rates, as well as increased payment for pediatric care from commercial payors.9
2024 Average Compensation: Adult vs. Pediatric Specialists
Pediatric Compensation Concerns
Most Pediatricians, Pediatric Subspecialists Report Inadequate Pay
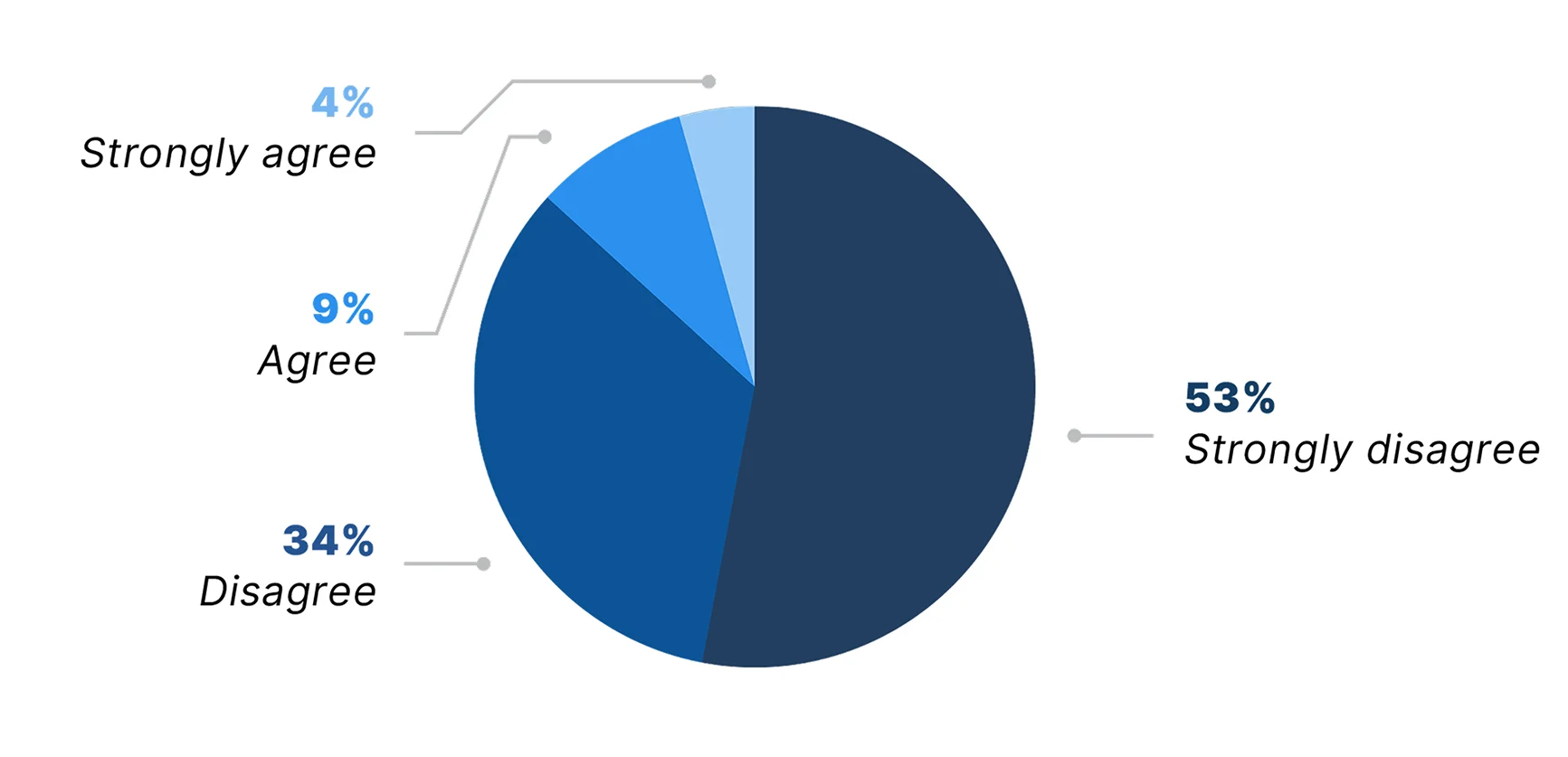
In June 2025, Doximity surveyed more than 1,200 pediatricians and pediatric subspecialists to better understand their views on compensation and reimbursement—and how these factors are impacting their work, their field, and patient care. The vast majority (87%) said they are not fairly compensated relative to the complexity and importance of their work.
The relatively lower compensation (compared with adult medicine specialists) has affected the ability of 87% of the physicians surveyed to repay their educational debt, save for retirement, or meet other financial goals. In addition, 69% said that relatively lower pay has led them to consider making a career change, including 23% who said they already have or plan to make a career change.
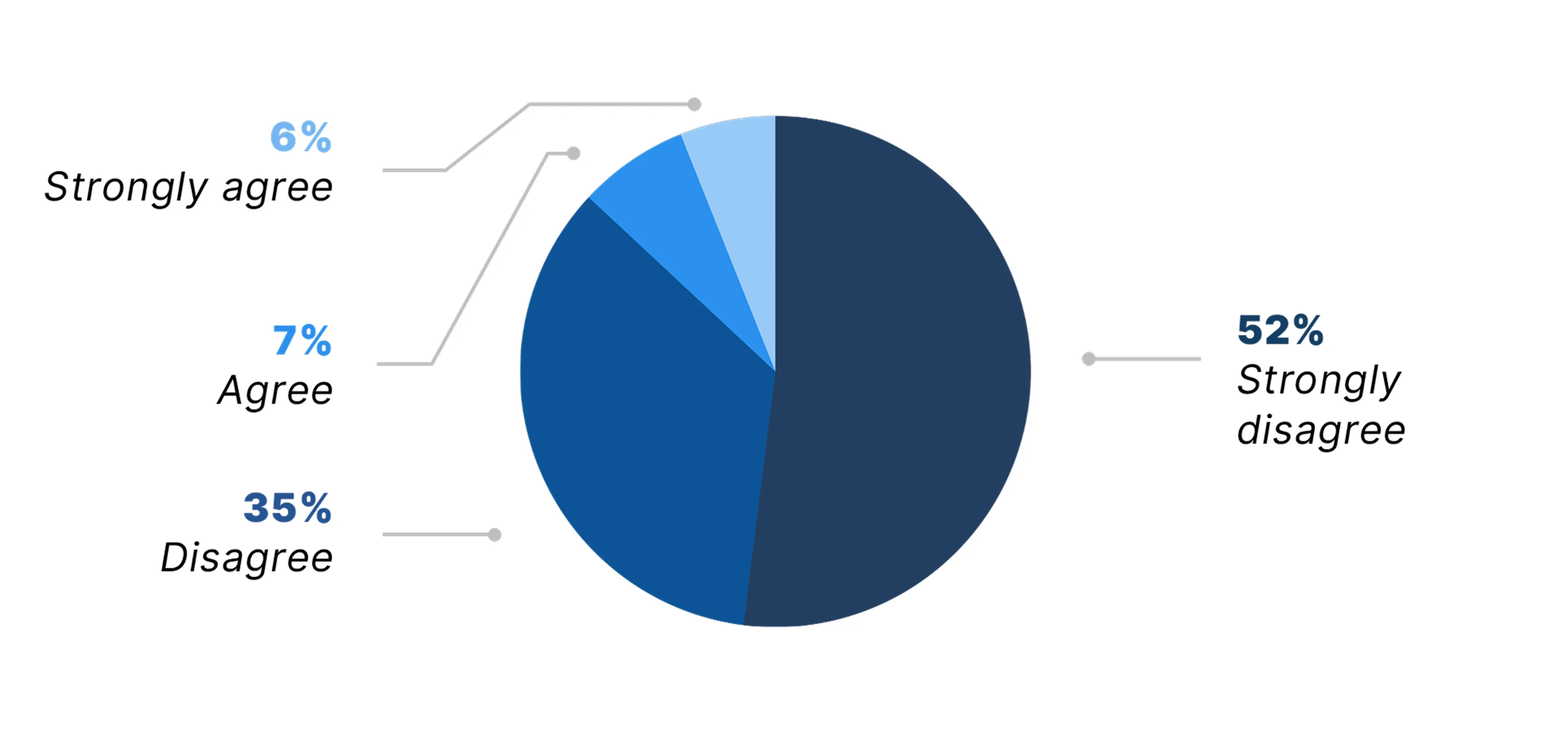
Pediatricians and pediatric specialists are fairly compensated relative to the complexity and importance of their work.
The comparatively lower compensation in pediatric care (compared with adult specialties) has affected my ability to repay educational debt, save for retirement, or meet other financial goals.*
*Due to rounding, numbers may not sum to 100%
Pediatric Reimbursement Challenges
Physicians Say Reimbursement Levels Limit, Interfere with Pediatric Patient Care
In addition to insufficient pay, current reimbursement levels in pediatrics and pediatric subspecialties also appear to fall short of patients’ needs. When asked whether reimbursement levels adequately align with the needs and complexity of today’s pediatric patient population, 87% of physicians surveyed said they disagree or strongly disagree.
Indeed, half of physicians surveyed (50%) said current reimbursement limits their ability to provide care for their pediatric patients, while another 37% said they are worried it could limit care in the future. The strong majority of all physicians surveyed (91%) said they are concerned that current reimbursement levels are interfering with early intervention and prevention efforts in pediatric care.
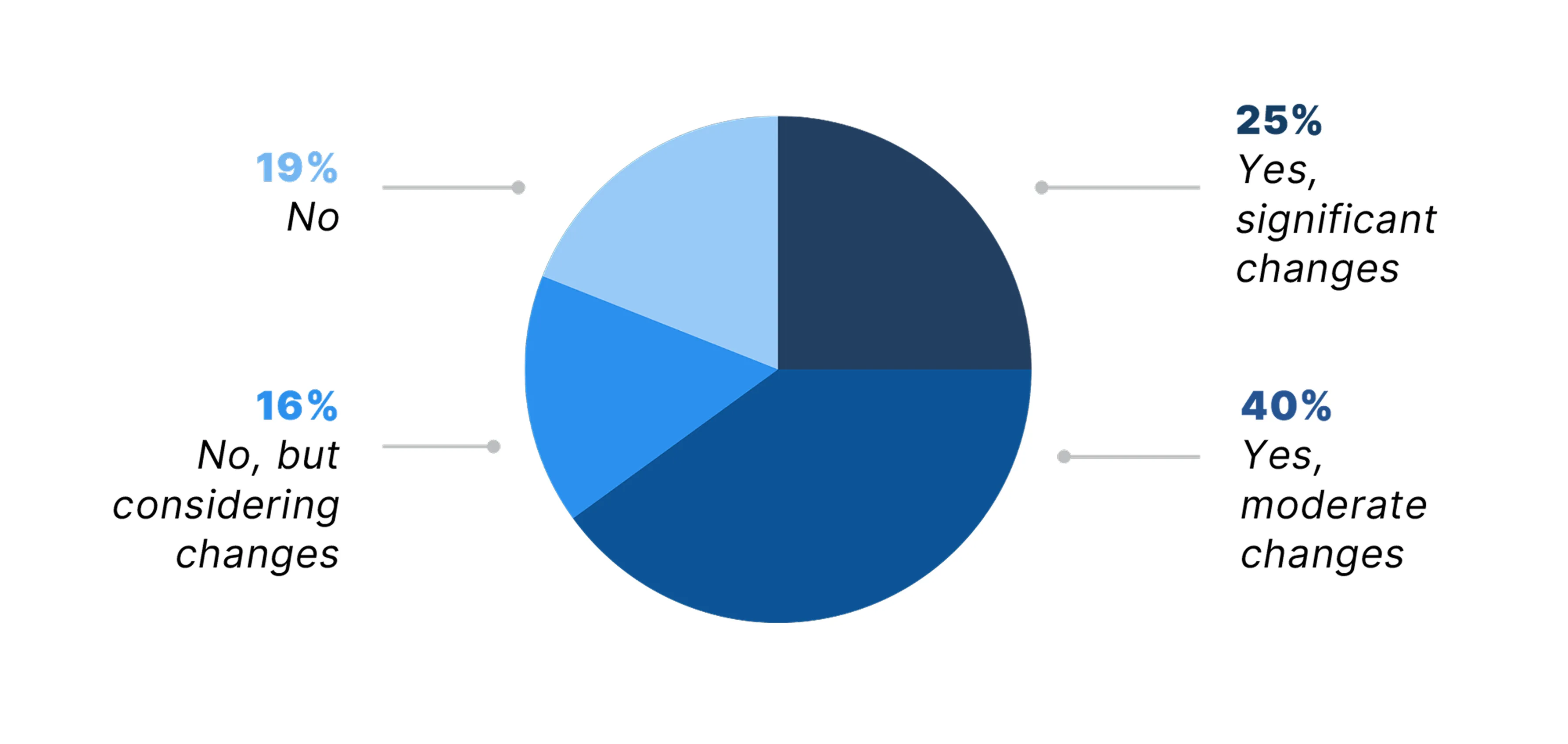
As a result of these financial pressures, 65% of the pediatricians and pediatric subspecialists reported they have had to make moderate or significant changes to their practice model—from increasing patient volume to reducing services or staff.
Current reimbursement levels adequately align with the needs and complexity of today's pediatric patient population.
Have you had to alter your practice model (e.g., increase patient volume, limit services, or reduce staff) due to financial pressures specific to pediatric care?
Impact on Recruitment and Retention
Pediatric Reimbursement Gap Hinders Recruitment, Retention
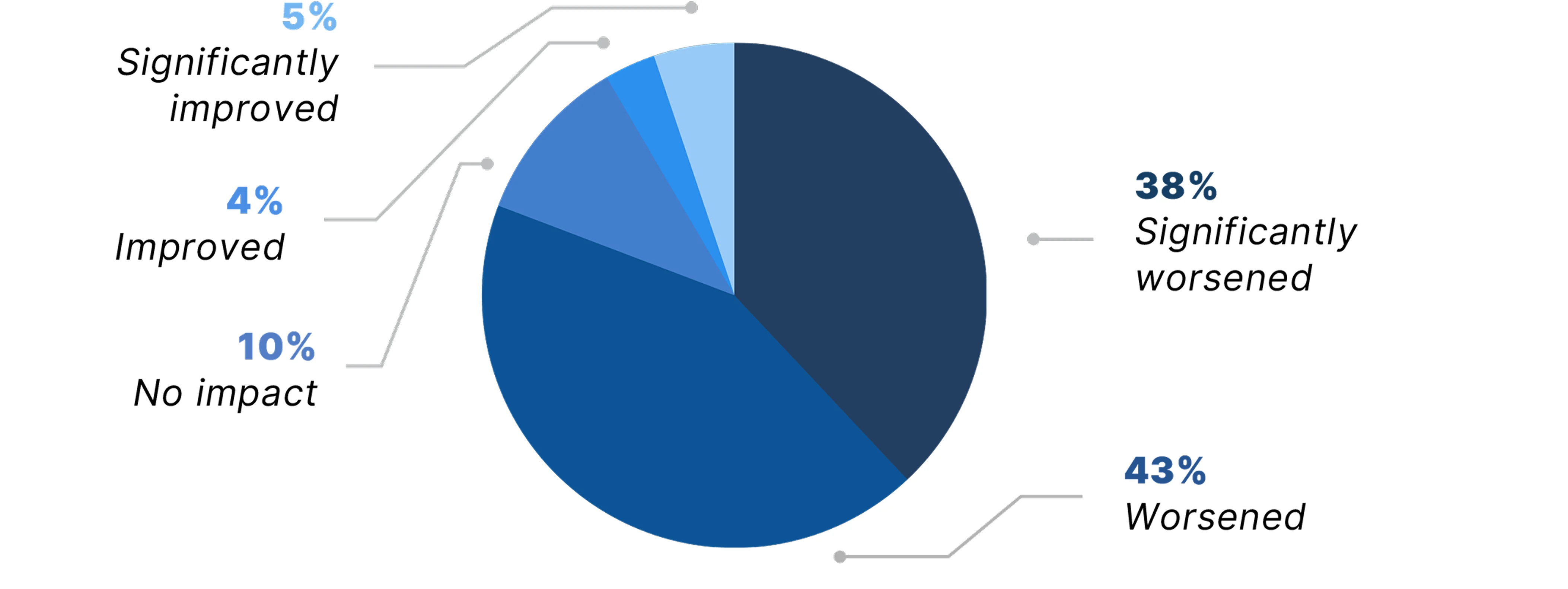
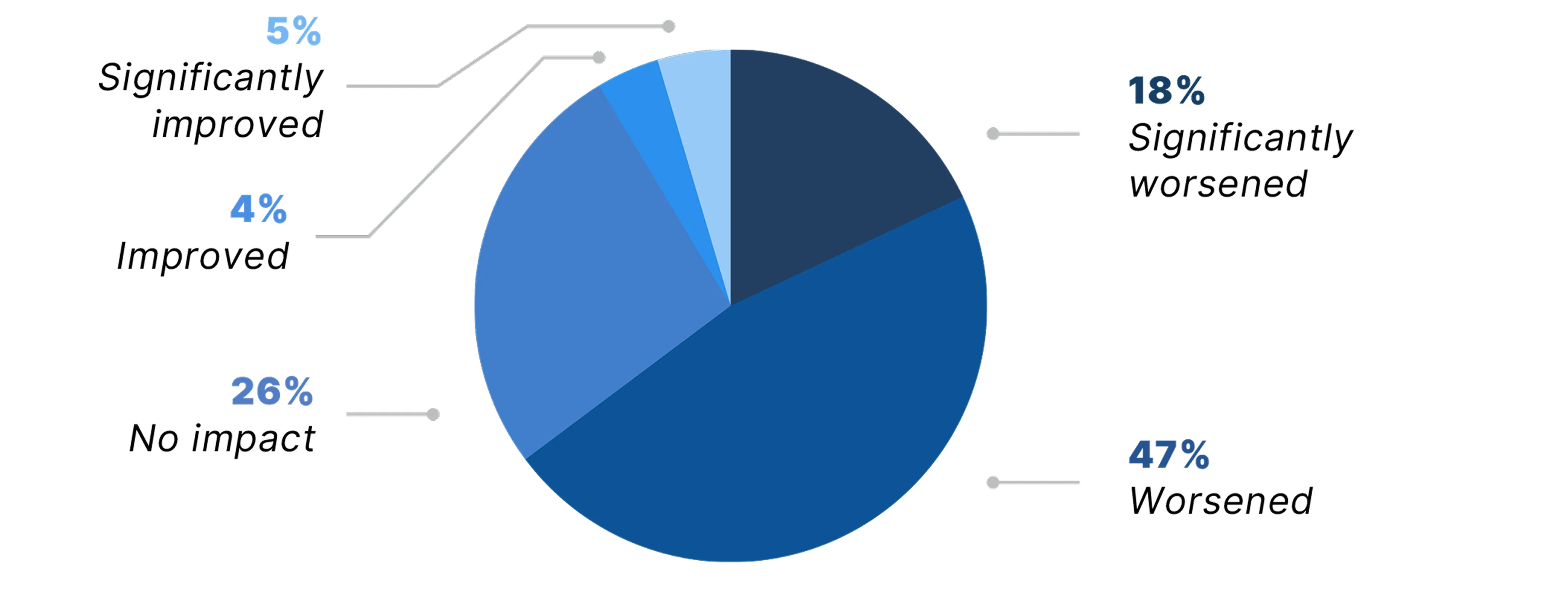
Compounding the issue, lower reimbursement in pediatrics and pediatric subspecialties appears to be negatively impacting physician recruitment and retention in these fields. More than 80% of pediatricians and pediatric subspecialists surveyed said the reimbursement gap between pediatrics and adult care has worsened or significantly worsened physician recruitment in their field. Similarly, more than 65% reported that the reimbursement gap has worsened or significantly worsened physician retention. This growing strain on recruitment and retention could further exacerbate the current pediatric workforce shortage.10
How has the reimbursement gap between pediatrics and adult care impacted physician recruitment in your field?
How has the reimbursement gap between pediatrics and adult care impacted physician retention in your field?
Opportunities for Improvement
Physicians Report Reimbursement Parity Would Have a Positive Impact on Patient Care
When asked which policy or reimbursement changes would have the greatest positive impact on pediatric care, 67% of pediatricians and pediatric subspecialists selected reimbursement parity between pediatric and adult care. This was followed by higher Medicaid reimbursement rates for pediatric services (61%) and better coverage for non-billable but essential services such as care coordination (51%).
These responses suggest that many physicians see current reimbursement structures as falling short in supporting pediatric care. Addressing these areas could support efforts to improve the pediatric workforce and access to care for children.

Which policy or reimbursement changes would have the greatest positive impact on pediatric care?*
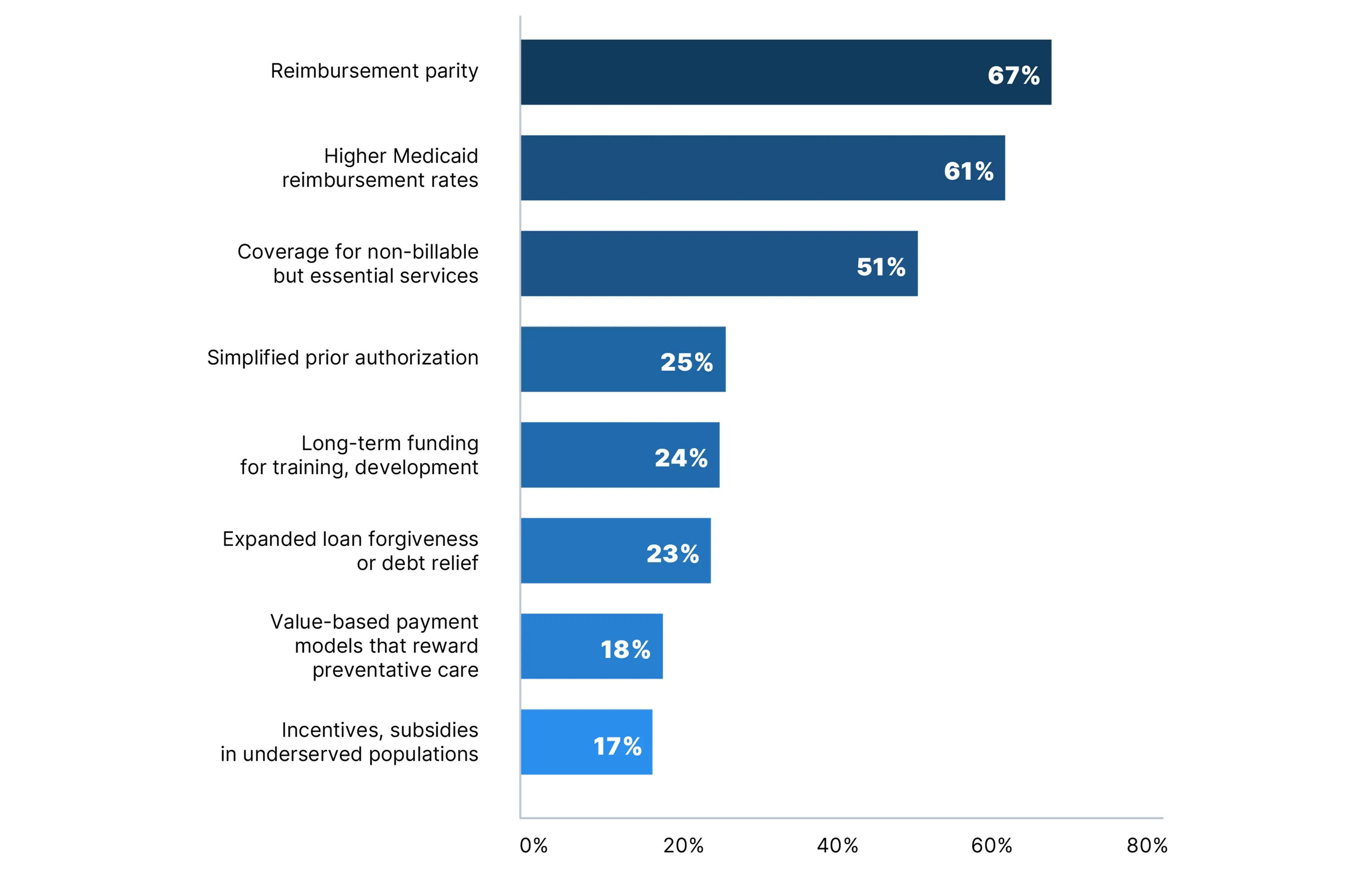
*Physician respondents selected up to 3
Commitment to Pediatric Care
Most Pediatricians, Pediatric Subspecialists Inspired to Stay in Their Field
Despite significant financial and systemic pressures, survey findings highlight the deep commitment many pediatricians and pediatric subspecialists feel toward their work. Nearly three-fourths (74%) of physicians surveyed said they are inspired to stay in pediatric care by their passion for their specialty or clinical focus, and a similar share cited a strong sense of purpose or mission in caring for children. In addition, 58% said they are motivated by the opportunity to build long-term relationships with both patients and their families.
These responses are a powerful reminder that, even in the face of serious challenges, it is dedication to children and their futures that keeps so many pediatricians and pediatric subspecialists in this vital field.
Despite potential financial or systemic pressures, what inspires you to stay in pediatric care?*
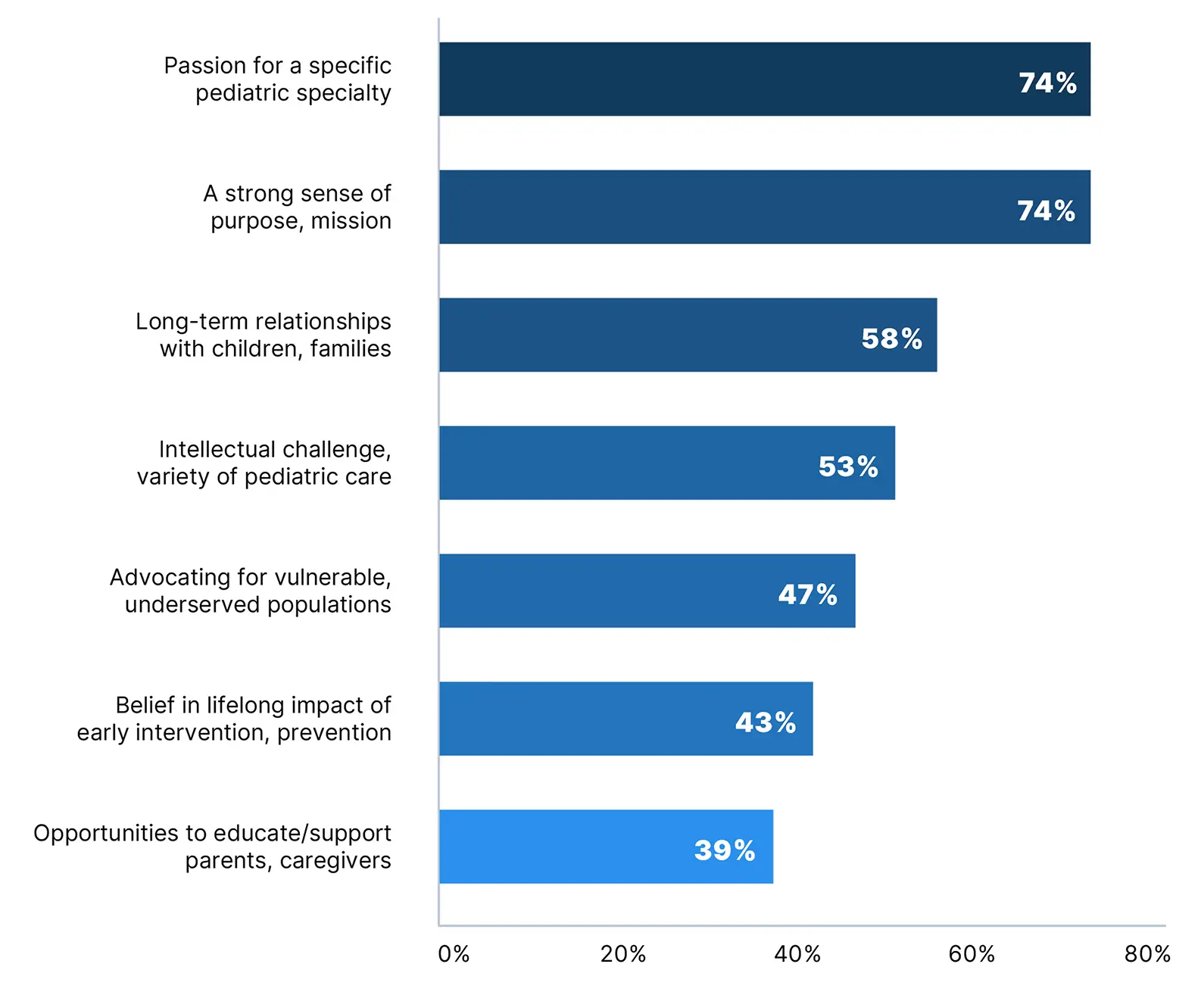
*Physician respondents selected all that applied
Reimbursement and Private Practice
Physicians Balance Reimbursement Challenges and Patient Commitment
Despite Reimbursement Challenges, the Majority of Physicians Remain Committed to Serving Medicare and Medicaid Patients
In June 2025, Doximity surveyed over 1,100 U.S. physicians across specialties to better understand the impact of declining reimbursement on patient care and private practice. Among physicians surveyed, 17% said they or their organization reduced the number of Medicare or Medicaid patients they see in the past 12 months due to reimbursement concerns, while another 13% said they are likely to do so in the future. Three percent (3%) reported they hadn’t seen Medicare or Medicaid patients at all during that time.
These findings indicate that nearly one-third of physicians surveyed have already reduced the number of Medicare and Medicaid patients they see or may need to do so in the future—underscoring the difficult choices many face as reimbursement pressures continue to grow. Still, the majority of physicians (53%) said they have not made any reductions and are not likely to, reflecting ongoing physician commitment to these patient populations.
In the past 12 months, have you or your organization reduced the number of Medicare or Medicaid patients you see due to reimbursement concerns?*
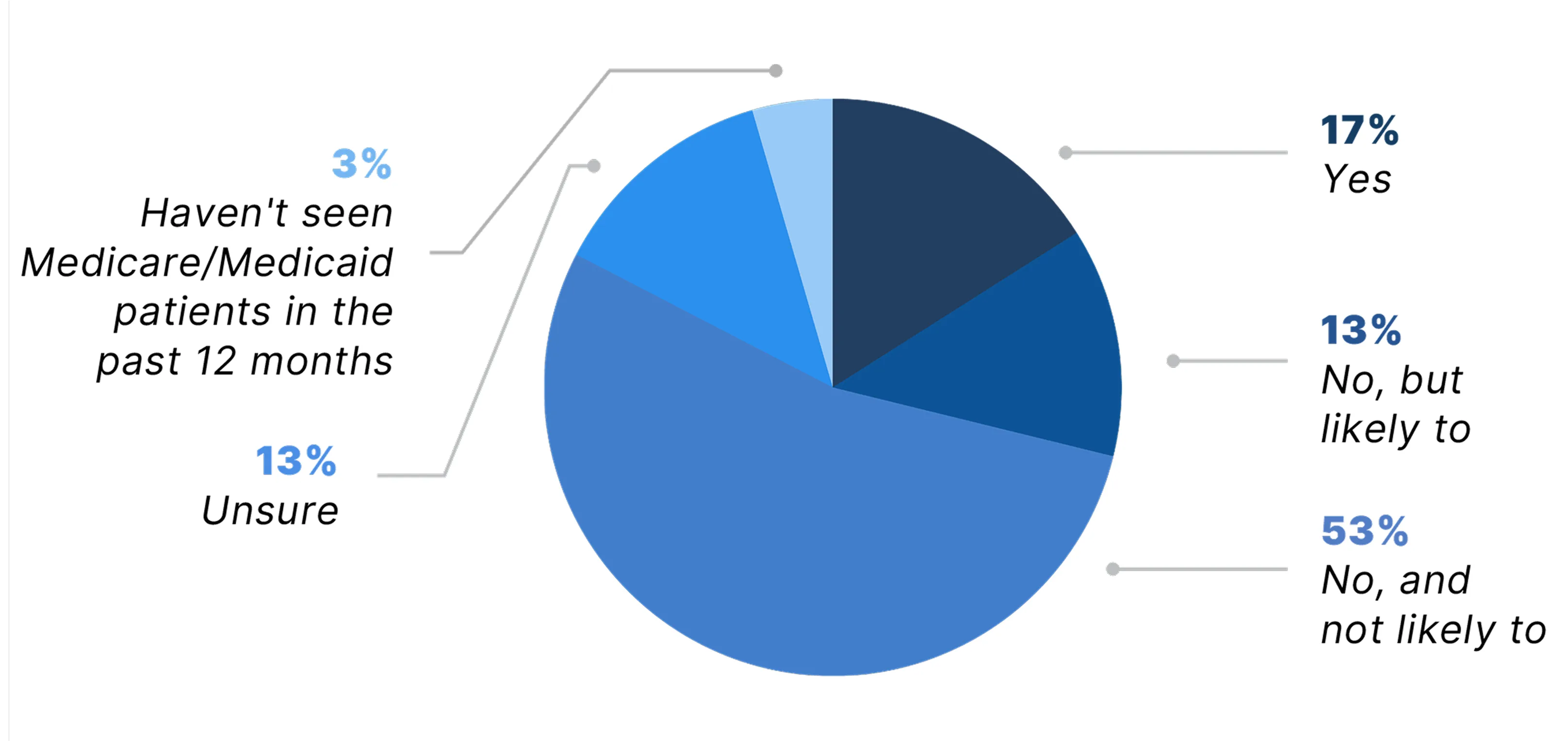
*Due to rounding, numbers may not sum to 100%
Physician Concerns About the Future of Medicare and Medicaid
Most Physicians Worry Reimbursement Pressures Could Affect Their Ability to Care for Medicare and Medicaid Patients
While most physicians surveyed said they do not expect to reduce the number of Medicare or Medicaid patients they see, the majority were concerned about their ability to serve these patients moving forward. Nearly 60% of physicians surveyed said they are either concerned (36%) or very concerned (24%) that reimbursement pressures will affect their ability to care for Medicare and Medicaid patients in the next 12 months.
These findings further reflect the difficult environment physicians are navigating as they strive to maintain access to care for Medicare and Medicaid patients amid reimbursement challenges.
Are you concerned that, in the next 12 months, reimbursement pressures will affect your ability to serve Medicare or Medicaid patients?*
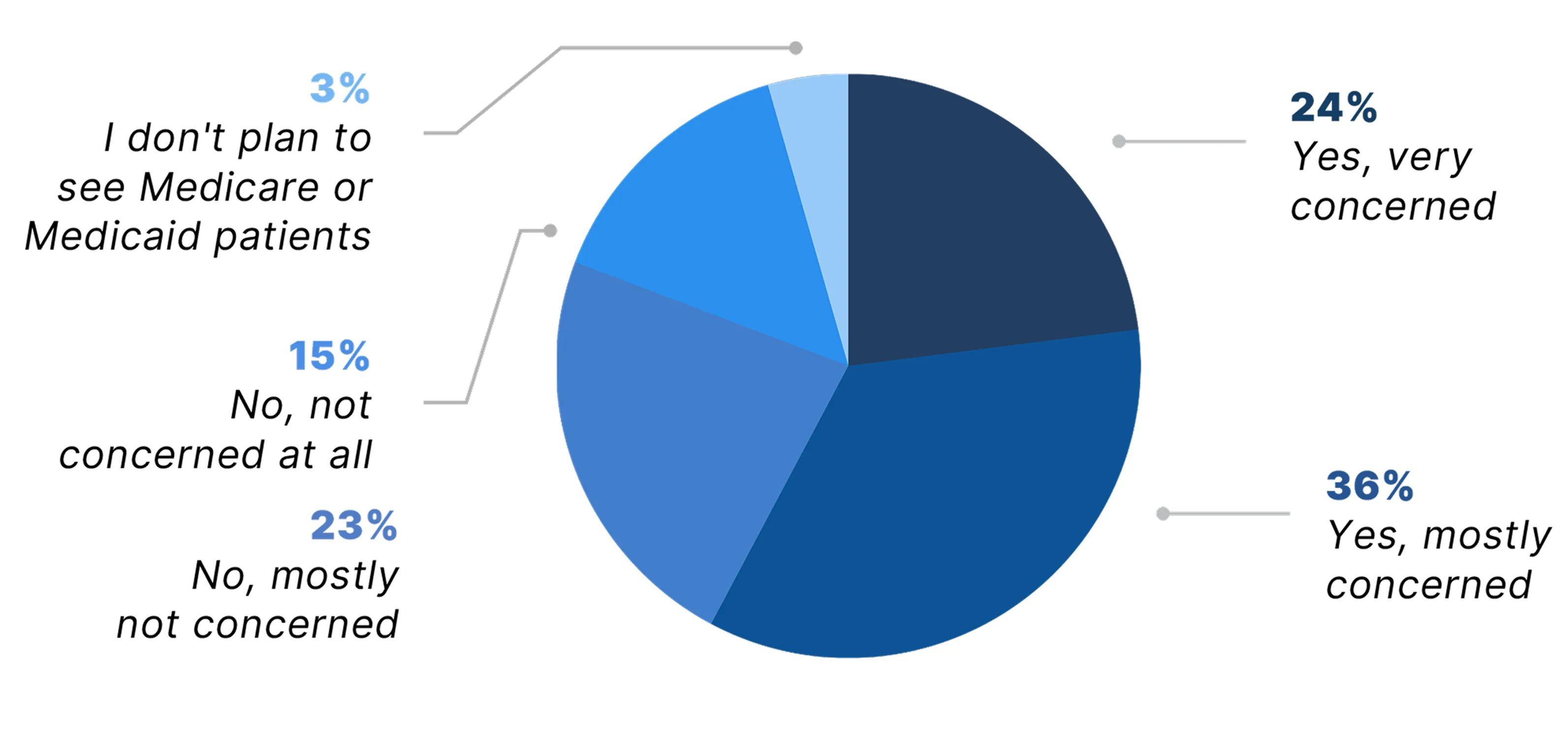
*Due to rounding, numbers may not sum to 100%
Impact on Practice Growth and Hiring Plans
More Than One-Third of Physicians Have Delayed or Canceled Plans to Hire Staff or Expand Services
Alongside growing concern about the future of Medicare and Medicaid patient care, physicians also reported that reimbursement pressures are limiting opportunities to strengthen or grow their practices. Nearly 38% said they or their organization had delayed or canceled plans to hire staff or expand services in the past 12 months because of reimbursement concerns. Another 19% said they are considering or planning to take such steps in the near future.
Of note, about one in five physicians (21%) said they were unsure whether their organization had delayed or canceled plans to hire or expand services, which may reflect not only the complexity of these decisions, but also the fact that many physicians today are employees rather than practice owners, with less direct control or visibility into these choices. The combination of delayed hiring, stalled service expansion, and fewer physicians at the decision-making table paints a concerning picture.
In the past 12 months, has your organization delayed or canceled plans to hire staff or expand services due to reimbursement concerns?*
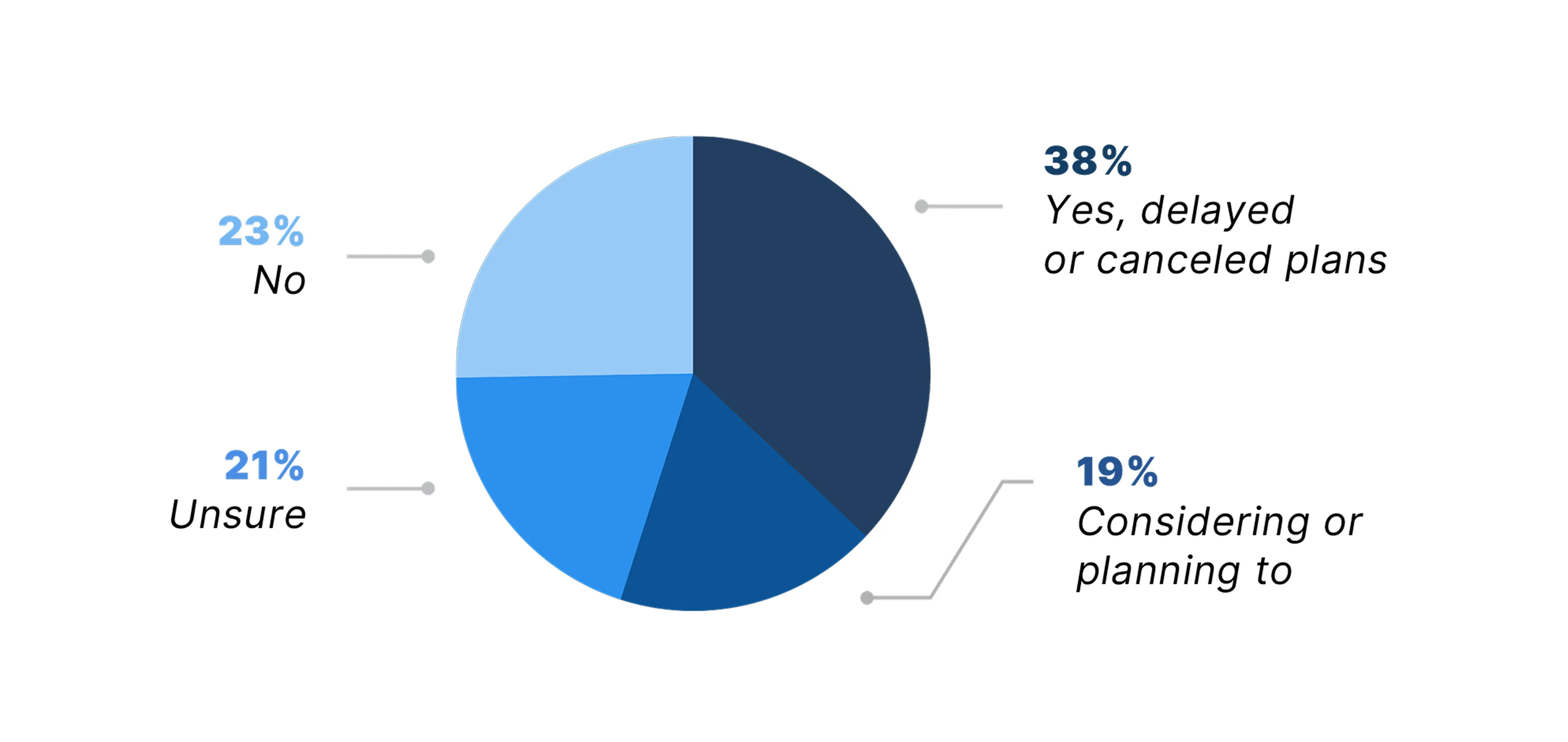
*Due to rounding, numbers may not sum to 100%
Reimbursement Policy and the Decline of Private Practice
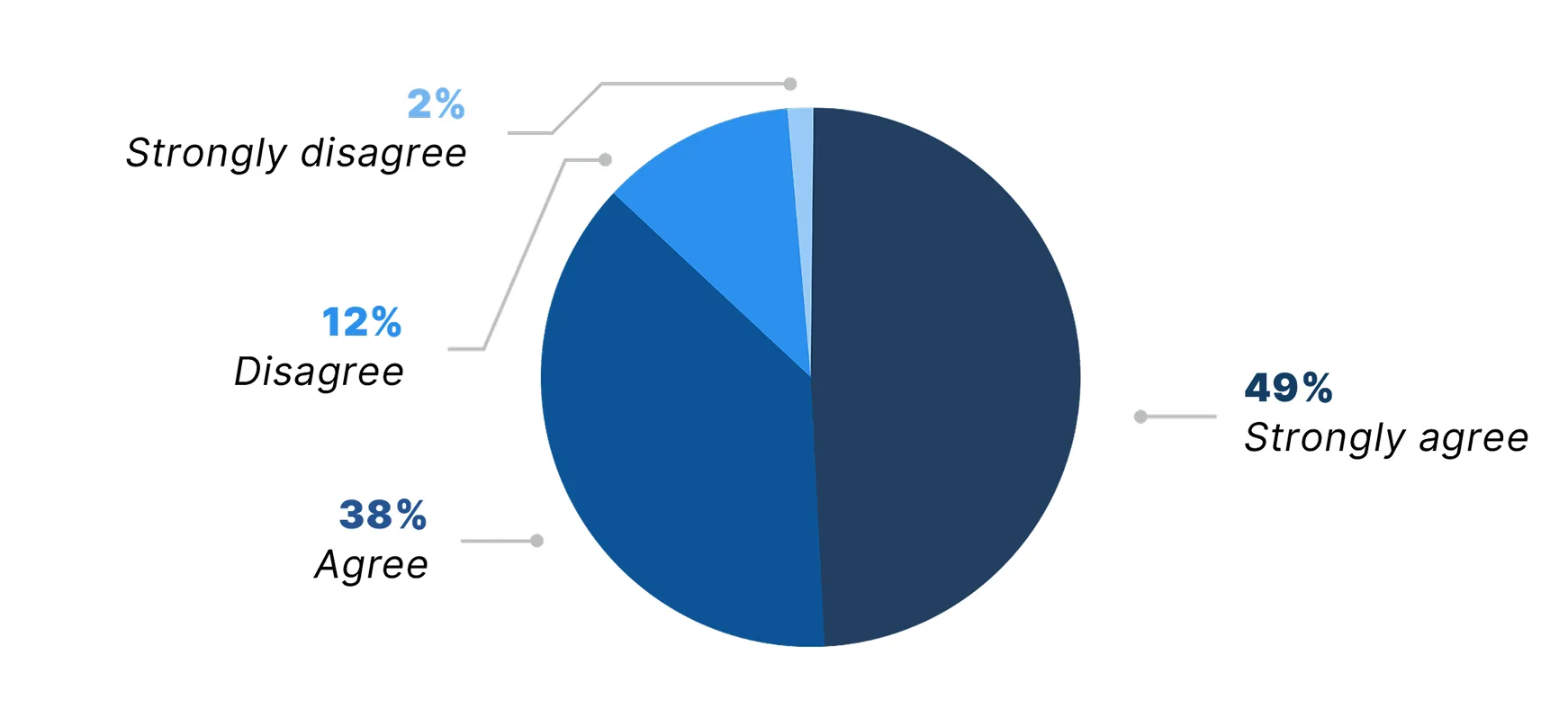
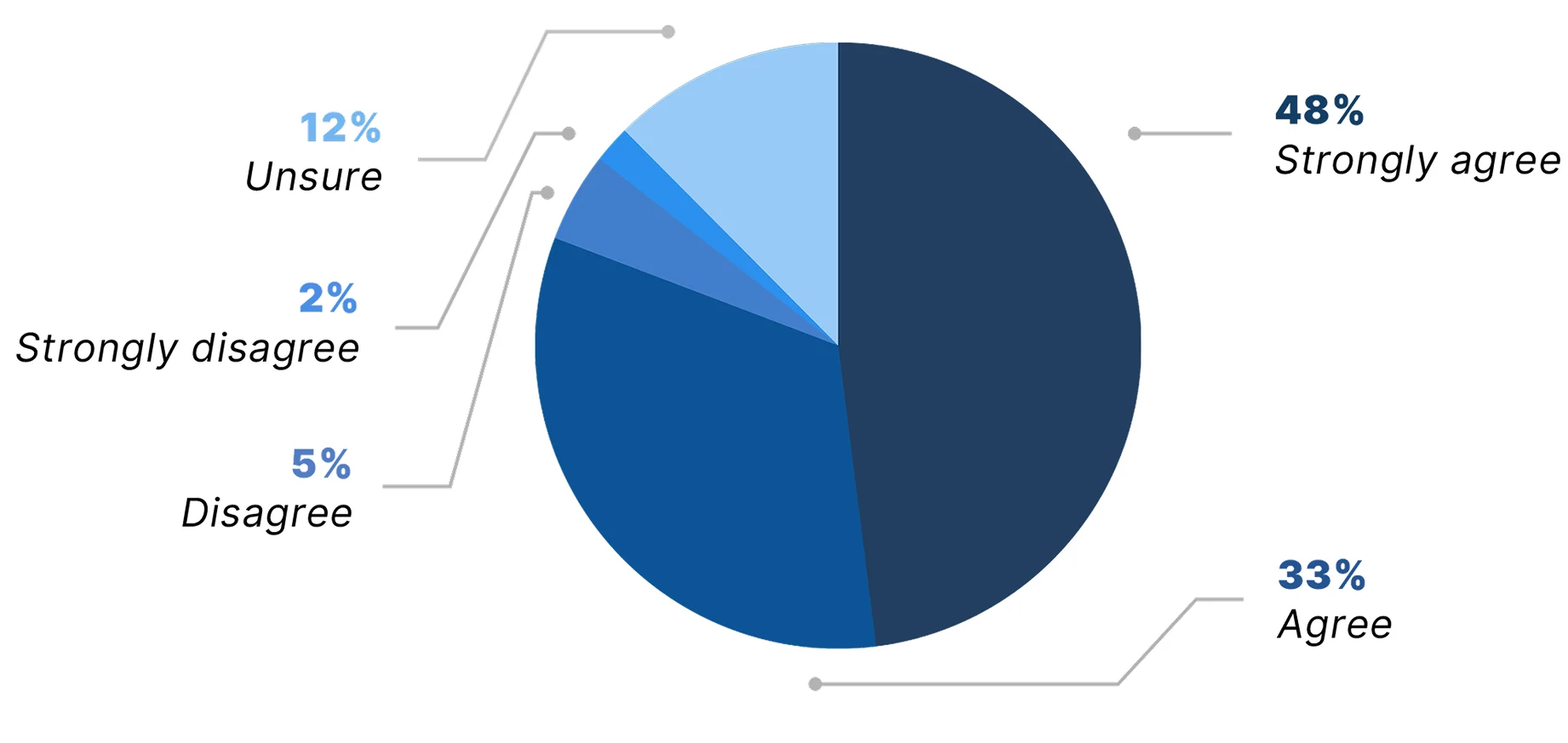
Eight in Ten Physicians Agree Reimbursement Policy Has Played Significant Role in the Decline of Independent Practice
Many physicians view current reimbursement policy as a key contributor to the decline of private practices. Among physicians surveyed, 81% agreed (33%) or strongly agreed (48%) that reimbursement policy has played a significant role in the decline of independent practices in their field. Just 7% of physicians disagreed.
According to the American Medical Association, private practices have been on the decline for years. Between 2012 and 2024, the share of physicians working in private practices dropped by 18 percentage points—from 60.1% to 42.2%.1
Reimbursement policy has played a significant role in the decline of independent practices in my field.
Physician Shortage, Demand, and Overwork
Physician Shortage
Majority of Physicians Report Being Negatively Affected by the Physician Shortage
The medical community faces a significant physician shortage projected to reach 86,000 physicians by 2036, according to the Association of American Medical Colleges (AAMC).11 More recent estimates by the U.S. Health Resources and Services Administration are even higher, anticipating a shortage of 187,130 full-time equivalent physicians by 2037.12
Among more than 1,100 U.S. physicians surveyed, 89% said their clinical practice has been affected by the shortage. Nearly 21% described it as “severe,” and many reported significant strain due to the shortage, including burnout, overwork, and lower job satisfaction. Moreover, more physicians than last year reported an inability or limited ability to accept new patients, suggesting workforce constraints continue to limit patient access.
That said, the intensity of negative experiences appears to have eased slightly year over year. It's possible that after years of pressure, physicians may be adjusting expectations, reducing hours, or pursuing more flexible practice models.
How would you describe the impact of the physician shortage in your clinical practice?*
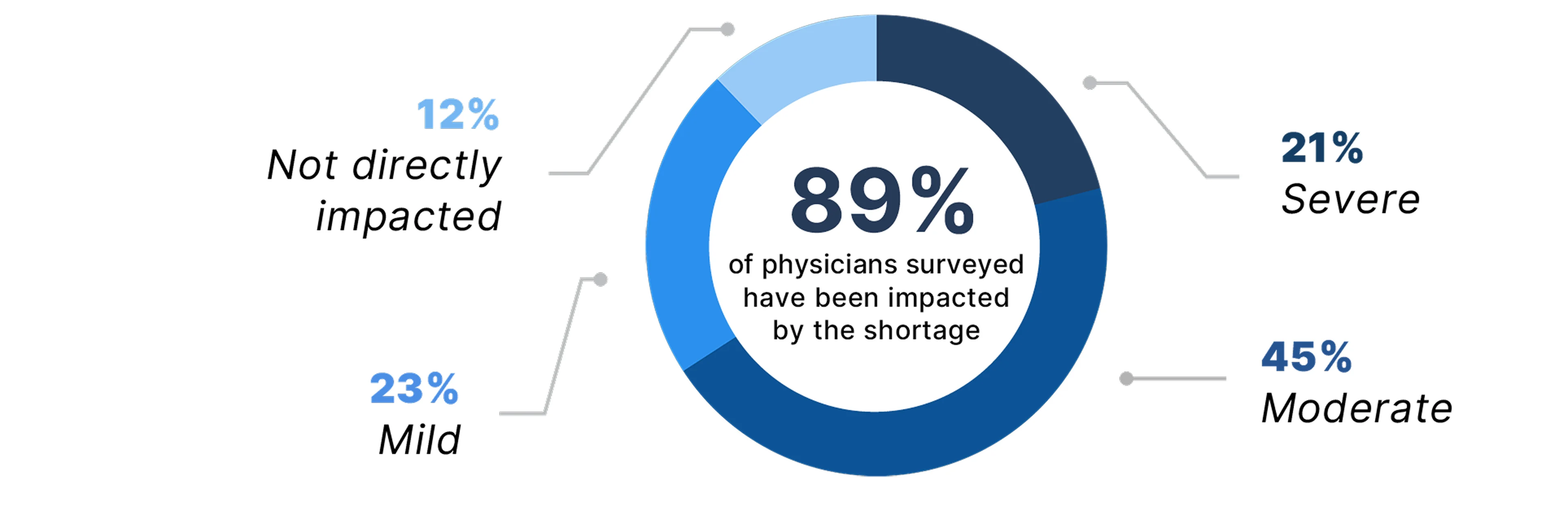
*Due to rounding, numbers may not sum to 100%
Which of the following have you personally experienced as a result of the physician shortage?†
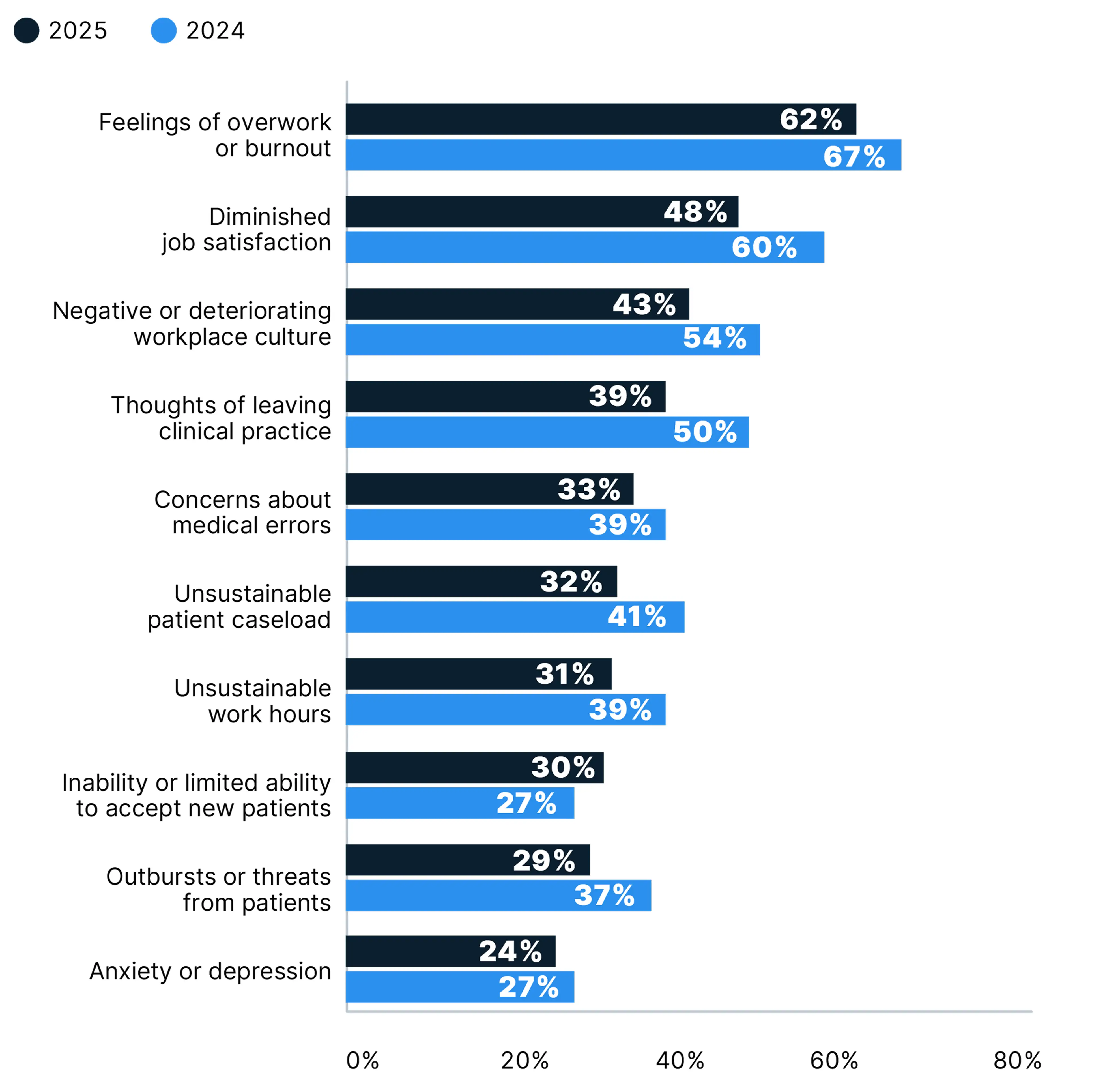
† Respondents selected all that applied
Impact of Overwork on Physician Career Plans
Most Physicians Report Being Overworked, Looking for an Employment Change
According to a multiyear report published in Mayo Clinic Proceedings, roughly half of physicians reported feeling burnout since at least 2011, with workforce shortages and overwork contributing to this trend.13,14 In a Doximity poll of nearly 2,000 physicians conducted in May 2025, 85% reported they are overworked, compared with 81% in 2023, 86% in 2022, and 73% in 2021. As a result, about 68% of physicians said they are looking for an employment change or considering early retirement.
Overwork appears to be especially prevalent among women physicians: 91% of women respondents reported being overworked, compared with 80% of men. This overwork has compelled 74% of women to consider making a career change, compared with 62% of men. There were differences among physician specialties as well: 90% of primary care physicians said they are overworked, compared with 84% of surgeons and 83% of non-surgical specialists.
How has your clinical workload altered your career plans?*
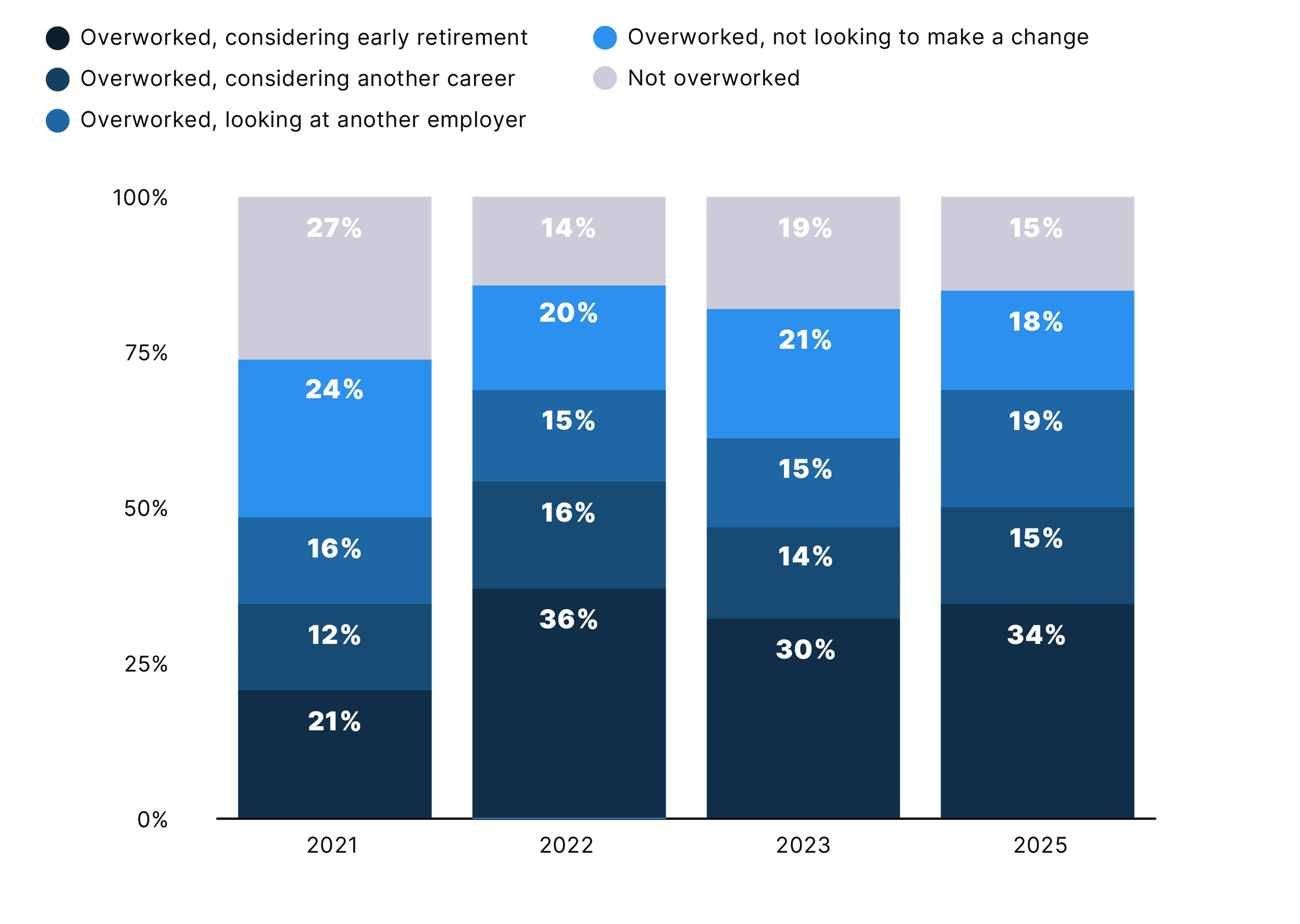
*Due to rounding, numbers may not sum to 100%
Importance of Autonomy and Work-Life Balance
Physicians More Willing to Accept Lower Pay for More Autonomy, Work-Life Balance
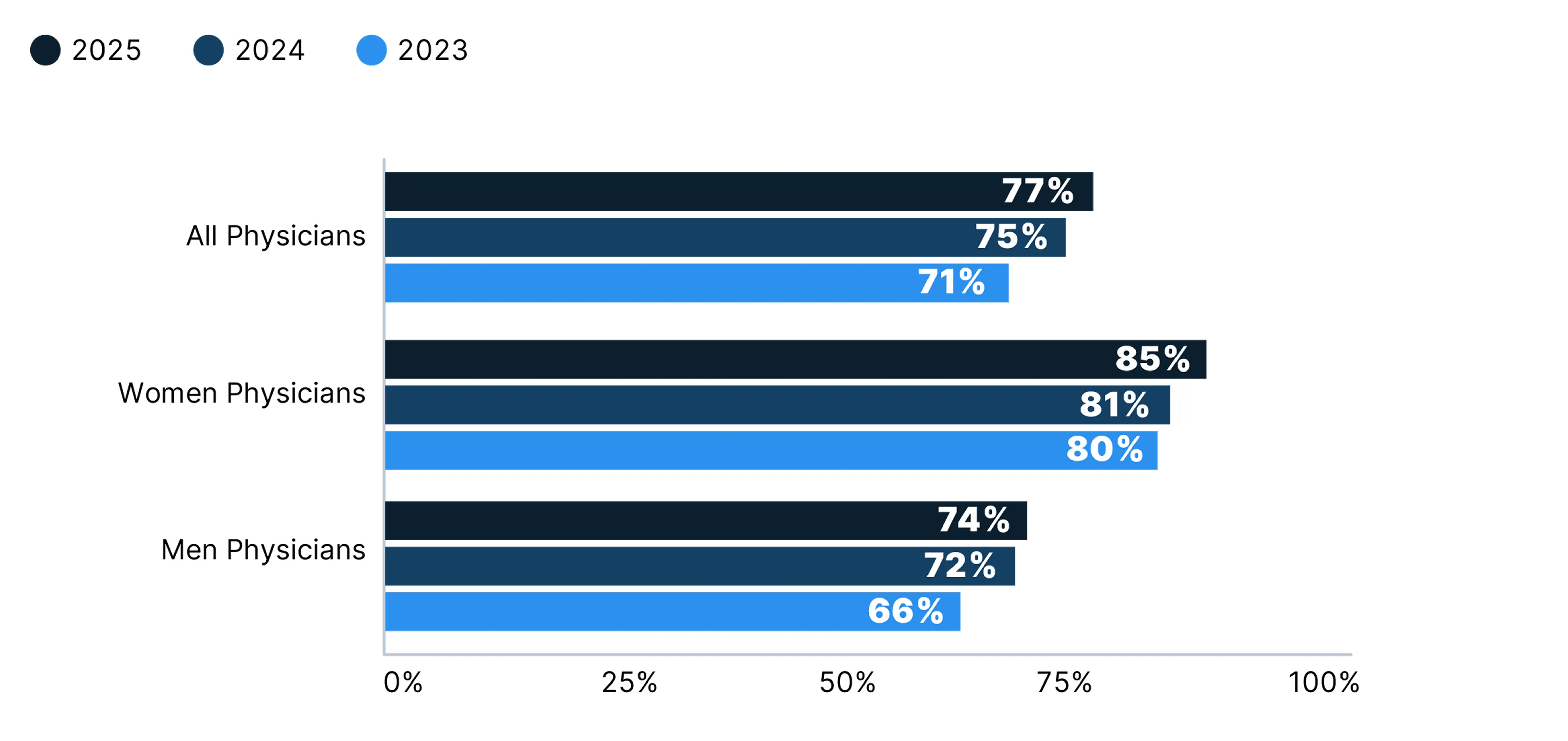
With the vast majority of physicians still feeling overworked, many have expressed a willingness to accept lower compensation if it would bring them greater autonomy or work-life balance. In another Doximity poll of nearly 2,000 physicians conducted in June 2025, 77% reported they would be willing to accept, or have already accepted, lower compensation to achieve more autonomy or work-life balance. This is a slight step up from 75% in 2024 and 71% in 2023.
On average, a higher percentage of women physicians (85% of women respondents) reported they would be willing to accept lower compensation for more autonomy or work-life balance than men physicians (74%)—consistent with prior years.
Percentage of Physicians Who Have Accepted, or Would Accept, Lower Compensation For More Autonomy or Work-Life Balance
Physician Demand by Specialty
Primary Care Specialties See the Most Demand
Amid concerns over an overstretched physician workforce, demand remains high across many medical specialties. The specialties that saw the highest demand in 2024 were predominantly primary care specialties, based on an analysis of tens of thousands of job postings across the Doximity network in 2024.
Three out of the four most recruited specialties were internal medicine, family medicine, and pediatrics. This high demand for primary care aligns with longstanding concerns over an anticipated shortage of 87,150 full-time equivalent primary care physicians by 2037, according to the U.S. Health Resources and Services Administration.15
Top 10 Specialties Based on Demand
| Specialty |
|---|
| 1. Internal Medicine |
| 2. Family Medicine |
| 3. Psychiatry |
| 4. Pediatrics |
| 5. Obstetrics & Gynecology |
| 6. Emergency Medicine |
| 7. Neurology |
| 8. General Surgery |
| 9. Anesthesiology |
| 10. Radiology |
Rise of Locum Tenens
Majority of Physicians Are Working in or Considering Locum Tenens
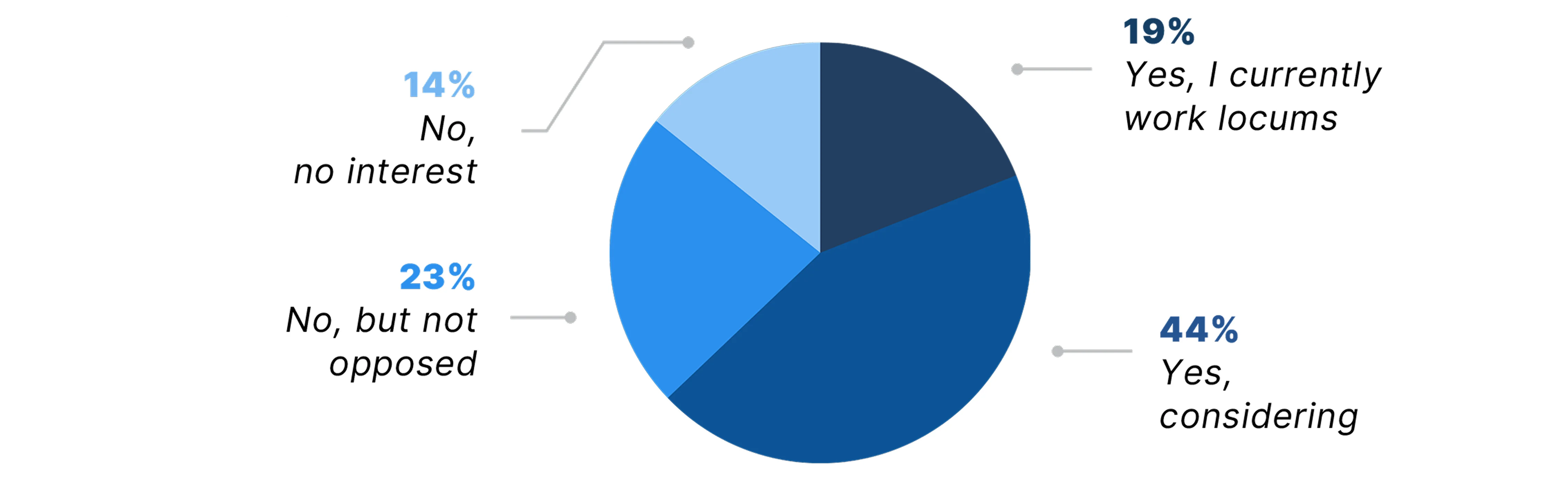
Beyond full-time work, locum tenens is an increasingly popular way for physicians to supplement their income or to practice with the benefits of reduced hours and more flexibility. More than 63% of physicians reported they are already working in locum tenens or considering taking on a locums role within the next five years, according to a Doximity poll of nearly 1,200 U.S. physicians.
Based on data from Doximity Talent Solutions, which supports both permanent and locum tenens staffing, the two specialties with the greatest demand for locum tenens work in 2024 were internal medicine and family medicine, both primary care specialties. The remainder of the top 10 most in-demand locums specialties included a mix of surgical and non-surgical specialties.
More than 63% of physicians surveyed are already working in locum tenens or considering it.
Top 10 Most In-Demand Locums Specialties
| Specialty |
|---|
| 1. Internal Medicine |
| 2. Family Medicine |
| 3. Obstetrics & Gynecology |
| 4. Anesthesiology |
| 5. Emergency Medicine |
| 6. Radiology |
| 7. Gastroenterology |
| 8. Psychiatry |
| 9. Oncology |
| 10. General Surgery |
Are You Considering Taking on a Locum Tenens Role in the Next Five Years?
Conclusion
Physicians today are navigating an increasingly complex and demanding landscape. They face a growing and aging patient population, workforce shortages, overwork and burnout, and reimbursement pressures, which collectively could worsen patient access to care. Yet despite these challenges, physicians remain deeply committed to caring for their patients and communities. In fact, 76% of physicians surveyed said that if they had the chance to do it over again, they would still choose to be a doctor.
But as we look ahead, questions remain: Are we relying too heavily on physicians rather than addressing the underlying need for policies and solutions that support a healthier, more sustainable future for all? Building that future will take more than physician dedication alone. It will require meaningful collaboration across the entire health care ecosystem—including health systems, hospitals, payors, and policymakers—and physicians must not only have a voice in shaping the path forward; they must have a seat at the table.
Methodology & Sources
Methodology
This study by Doximity was drawn from over 37,000 physician compensation surveys completed between January and December 2024, with data from over 230,000 compensation surveys over the last six years. Each survey was completed by full-time U.S. physicians who practice at least 40 hours per week. Responses were mapped across metropolitan statistical areas, and 60 of the top represented MSAs were included in the analysis.
To control for differences in specialty, geography, and other provider-specific factors, we estimated a multivariate regression with controls for provider specialty, metro area, and gender. We also controlled for how long each provider has practiced medicine and their self-reported average hours worked per week.
Cost of Living Adjustment
This analysis used the 2023 regional price parities of metropolitan statistical areas published by the Bureau of Economic Analysis. The price parities are publicly available in the December 12, 2024 release on the BEA website.
Pediatric Workforce and Compensation Survey
Doximity conducted a survey of pediatricians and pediatric subspecialists in June 2025 about the current state of compensation and reimbursement in their field. This survey was completed by over 1,200 U.S. physicians across a broad range of pediatric specialties, including general pediatrics, child neurology, pediatric cardiology, pediatric hematology and oncology, and other pediatric subspecialties. Survey participant demographics are not population-based. Therefore, findings may not be able to be extrapolated to the broader physician population.
Physician Workforce and Reimbursement Survey
Doximity conducted a survey of its physician membership in June 2025 about their career and compensation satisfaction as well as the impact of declining reimbursement on patient care and private practice. The survey was completed by more than 1,100 U.S. physicians across a broad range of medical specialties. Survey participant demographics are not population-based. Therefore, findings may not be able to be extrapolated to the broader physician population.
Physician Overwork Poll
Doximity’s findings are based on a poll run on the Doximity Newsfeed in May 2025. Nearly 2,000 U.S. physicians responded to the poll.
The poll asked the following question: “How has your clinical workload altered your career plans?”
The poll offered the following five answer options:
- “Because of overwork, I’m looking for another employer.”
- “Because of overwork, I’m looking at another career.”
- “Because of overwork, I’m considering early retirement.”
- “I am overworked, but not looking to change my employer.”
- “I am not overworked.”
Autonomy and Work-Life Balance Poll
Doximity’s findings are based on a poll run on the Doximity Newsfeed in June 2025. More than 1,800 U.S. physicians responded.
The poll asked the following question: “Would you be willing to accept lower compensation to achieve more autonomy or work-life balance?”
The poll offered the following five answer options:
- “Yes, and I have already done so.”
- “Yes, I would consider it.”
- “No, probably not.”
- “No, definitely not.”
- “Unsure.”
Physician Demand by Specialty
The findings are based on tens of thousands of unique jobs posted on the Doximity network between January 1 and December 31, 2024. The job postings originated from Doximity’s Talent Solutions, which supports both permanent and locum tenens recruitment.
Locum Tenens Poll
Doximity’s findings are based on a poll run on the Doximity Newsfeed in April and May 2025. Nearly 1,200 U.S. physicians responded to the poll.
The poll asked the following question: “Are you considering taking on a locum tenens role in the next five years?”
The poll offered the following four answer options:
- “Yes, and I currently work locum tenens.”
- “Yes, I'm considering locum tenens.”
- “No, but I'm not opposed to it.”
- "No, I have no interest in locum tenens."
References
- 1Physician Practice Benchmark Survey. American Medical Association.
- 2Consumer Price Index: 2024 in Review. U.S. Bureau of Labor Statistics.
- 32025 Medicare Physician Payment Schedule (PFS) and Quality Payment Program (QPP) Final Rule Summary. American Medical Association.
- 4Medicare Experts Back Tying Physician Payment to Inflation. American Medical Association.
- 5Responding to the Workforce Crisis: Consensus Recommendations from the Second Workforce Summit of the American Society of Pediatric Nephrology. Pediatric Nephrology. 2024 Jul;39:3609-3619.
- 6Obesity and Chronic Kidney Disease: Prevalence, Mechanism, and Management. Clinical and Experimental Pediatrics 2021;64(10):511-518.
- 7Child Health Needs and the Pediatric Nephrology Subspecialty Workforce: 2020–2040. Pediatrics. 2024;153(Supplement 2):e2023063678P.
- 8Whaley CM, Koo T, Arora VM, Ganguli I, Gross N, Jena AB. Female Physicians Earn An Estimated $2 Million Less Than Male Physicians Over A Simulated 40-Year Career. Health Affairs. 2021 Dec;40(12):1856-1864.
- 9Lakshminrusimha S, Chen TL, Leonard MB, Devaskar SU, Vinci RJ, Degnon L, St. Geme JW. Raising the Bar: The Need for Increased Financial Support to Sustain and Expand the Community of Pediatric Subspecialists. The Journal of Pediatrics. 2024 Apr;267:113758.
- 10Pediatric Workforce Shortages Persist in 2024. Children’s Hospital Association.
- 11The Complexities of Physician Supply and Demand: Projections From 2021 to 2036. Association of American Medical Colleges.
- 12Physician Workforce: Projections, 2022-2037. November 2024. U.S. Health Resources and Services Administration.
- 13Shanafelt TD, West CP, Sinsky C, Trockel M, Tutty M, Wang H, Carlasare LE, Dyrbye LN. Changes in Burnout and Satisfaction With Work–Life Integration in Physicians and the General US Working Population Between 2011 and 2023. Mayo Clinic Proceedings. 2025 Jul;100(7):1142-1158.
- 14Addressing Health Worker Burnout: The U.S. Surgeon General’s Advisory on Building a Thriving Health Workforce. 2022.
- 15State of the Primary Care Workforce. U.S. Health Resources and Services Administration.